SEDAJECT Dexmedetomidine hydrochloride injection, 0.5 mg/mL (Canada)
This treatment applies to the following species: Company: Grey Wolf Animal Health
Company: Grey Wolf Animal Health
Sedative/analgesic
Veterinary Use Only
DIN 02492431
Sterile
For IM or IV administration in dogs and cats
Description
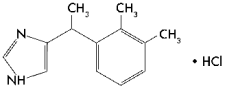
Sedaject (dexmedetomidine hydrochloride) is a synthetic alpha2-adrenoreceptor agonist with sedative and analgesic properties. The chemical name is (+)-4-[(S)-α, 2,3-trimethylbenzyl]imidazole hydrochloride. It is a white, or almost white, crystalline, water soluble substance having a molecular weight of 236.7. The molecular formula is C13 H16 N2 • HCl and the structural formula is:
Each mL of Sedaject contains 0.5 mg dexmedetomidine HCl, 1.6 mg methyl parahydroxybenzoate and 0.2 mg propyl parahydroxybenzoate as preservatives, 6.5 mg sodium chloride and water for injection.
SEDAJECT Dexmedetomidine hydrochloride injection, 0.5 mg/mL Indications
Sedaject is indicated for use as a sedative and analgesic in dogs and cats to facilitate clinical examinations, clinical procedures, minor surgical procedures, and minor dental procedures. Sedaject is also indicated for use as a preanesthetic to general anesthesia in dogs and cats.
Dosage and Administration
It is recommended that dogs and cats be fasted for 12 hours before treatment with Sedaject. An eye lubricant should be applied to prevent corneal desiccation that may occur during sedation. Following injection of Sedaject, the animal should be allowed to rest quietly for 15 minutes; sedation and analgesia occur within 5 to 15 minutes, with peak effects at 20 to 30 minutes after Sedaject.
Dogs: Sedaject produces sedation and analgesia when administered intramuscularly (IM) at a dose of 500 µg/m2, or intravenously (IV) at a dose of 375 µg/m2. Doses for preanesthesia are 125 or 375 µg/m2 IM. The choice of preanesthetic dose depends on the duration and severity of the procedure, as well as the anesthetic regime. The following two tables may be used to determine the correct dexmedetomidine HCl dosage. Note that the µg/kg dosage decreases as bodyweight increases. For example, dogs weighing 2 kg are dosed at 28 µg/kg dexmedetomidine hydrochloride IV, compared to dogs weighing 80 kg that are dosed at 9 µg/kg.
Due to the small volume of administration, accurate dosing is not possible in dogs weighing less than 2 kg.
TABLE 1:
SEDATION/ANALGESIA DOSE TABLE: Intravenous (IV) and intramuscular (IM) dosing on the basis of bodyweight:
|
Sedation/analgesia in dogs |
||||
|
Dog Weight (kg) |
Dexmedetomidine HCl 375 µg/m2 IV |
Dexmedetomidine HCl 500 µg/m2 IM |
||
|
µg/kg |
Sedaject mL |
µg/kg |
Sedaject mL |
|
|
2-3 |
28.1 |
0.12 |
40.0 |
0.15 |
|
3-4 |
25.0 |
0.15 |
35.0 |
0.20 |
|
4-5 |
23.0 |
0.20 |
30.0 |
0.30 |
|
5-10 |
19.6 |
0.29 |
25.0 |
0.40 |
|
10-13 |
16.8 |
0.38 |
23.0 |
0.50 |
|
13-15 |
15.7 |
0.44 |
21.0 |
0.60 |
|
15-20 |
14.6 |
0.51 |
20.0 |
0.70 |
|
20-25 |
13.4 |
0.60 |
18.0 |
0.80 |
|
25-30 |
12.6 |
0.69 |
17.0 |
0.90 |
|
30-33 |
12.0 |
0.75 |
16.0 |
1.00 |
|
33-37 |
11.6 |
0.81 |
15.0 |
1.10 |
|
37-45 |
11.0 |
0.90 |
14.5 |
1.20 |
|
45-50 |
10.5 |
0.99 |
14.0 |
1.30 |
|
50-55 |
10.1 |
1.06 |
13.5 |
1.40 |
|
55-60 |
9.8 |
1.13 |
13.0 |
1.50 |
|
60-65 |
9.5 |
1.19 |
12.8 |
1.60 |
|
65-70 |
9.3 |
1.26 |
12.5 |
1.70 |
|
70-80 |
9.0 |
1.35 |
12.3 |
1.80 |
|
>80 |
8.7 |
1.42 |
12.0 |
1.90 |
TABLE 2:
PREANESTHESIA DOSE TABLE: Intramuscular (IM) dosing on the basis of bodyweight:
|
Preanesthesia in dogs |
||||
|
Dog Weight (kg) |
Dexmedetomidine HCl 125 µg/m2 IM |
Dexmedetomidine HCl 375 µg/m2 IM |
||
|
µg/kg |
Sedaject mL |
µg/kg |
Sedaject mL |
|
|
2-3 |
9.4 |
0.04 |
28.1 |
0.12 |
|
3-4 |
8.3 |
0.05 |
25.0 |
0.15 |
|
4-5 |
7.7 |
0.07 |
23.0 |
0.20 |
|
5-10 |
6.5 |
0.10 |
19.6 |
0.29 |
|
10-13 |
5.6 |
0.13 |
16.8 |
0.38 |
|
13-15 |
5.2 |
0.15 |
15.7 |
0.44 |
|
15-20 |
4.9 |
0.17 |
14.6 |
0.51 |
|
20-25 |
4.5 |
0.20 |
13.4 |
0.60 |
|
25-30 |
4.2 |
0.23 |
12.6 |
0.69 |
|
30-33 |
4.0 |
0.25 |
12.0 |
0.75 |
|
33-37 |
3.9 |
0.27 |
11.6 |
0.81 |
|
37-45 |
3.7 |
0.30 |
11.0 |
0.90 |
|
45-50 |
3.5 |
0.33 |
10.5 |
0.99 |
|
50-55 |
3.4 |
0.35 |
10.1 |
1.06 |
|
55-60 |
3.3 |
0.38 |
9.8 |
1.13 |
|
60-65 |
3.2 |
0.40 |
9.5 |
1.19 |
|
65-70 |
3.1 |
0.42 |
9.3 |
1.26 |
|
70-80 |
3.0 |
0.45 |
9.0 |
1.35 |
|
>80 |
2.9 |
0.47 |
8.7 |
1.42 |
The use of Sedaject as a preanesthetic markedly reduces anesthetic requirements. Injectable induction drug requirements for intubation will be reduced between 30% and 60%, depending on the choice of anesthetic and the Sedaject preanesthetic dose. The concentration of inhalation maintenance anesthetic will be reduced between 40% and 60%, depending on the dose of Sedaject.
The anesthetic dose should always be titrated against the response of the patient. The choice of anesthetic is left to the discretion of the veterinarian.
Cats: Sedaject produces sedation and analgesia when administered IM at a dose of 40 µg/kg. This dose can also be used as a preanesthetic and has been shown to reduce anesthetic requirements in cats. Injectable anesthetic drug requirements for intubation were reduced up to 49%, depending on the choice of induction drug. The concentration of inhalation maintenance anesthetic was reduced between 35% and 44%, depending on the choice of induction drug. The anesthetic dose should always be titrated against the response of the patient.
The following table may be used to determine the correct dexmedetomidine HCl dosage for cats based on bodyweight.
TABLE 3: SEDATION/ANALGESIA DOSE TABLE: Intramuscular (IM) dosing on the basis of bodyweight in cats:
|
Sedation/analgesia in cats |
||
|
Cat Weight (kg) |
Dexmedetomidine HCl 40 µg/kg IM |
|
|
µg/kg |
Sedaject mL |
|
|
1-2 |
40 |
0.1 |
|
2-3 |
40 |
0.2 |
|
3-4 |
40 |
0.3 |
|
4-6 |
40 |
0.4 |
|
6-7 |
40 |
0.5 |
|
7-8 |
40 |
0.6 |
|
8-10 |
40 |
0.7 |
Contraindications
Do not use Sedaject in dogs or cats with cardiovascular disease, respiratory disorders, liver or kidney diseases, or in conditions of shock, severe debilitation, or stress due to extreme heat, cold or fatigue. Do not use in cases of known hypersensitivity to the active substance or to any of the excipients.
CAUTIONS:
Sedaject in cats has not been evaluated in the presence of other sedatives.
Although not observed in the feline field studies with dexmedetomidine hydrochloride, rare cases of delayed pulmonary edema, some resulting in death, have been reported in cats that received dexmedetomidine hydrochloride. In these cases, dyspnea due to the delayed onset of pulmonary edema developed up to three days after Sedaject administration.
Sedaject should not be administered in the presence of preexisting hypotension, hypoxia, or bradycardia. Due to the pronounced cardiovascular effects of dexmedetomidine, only clinically healthy dogs and cats should be treated. Animals should be frequently monitored for cardiovascular function and body temperature during sedation or anesthesia.
An intramuscular atipamezole hydrochloride sterile injection may be routinely used to rapidly reverse the effects of Sedaject in dogs. Since analgesic as well as sedative effects will be reversed, pain management may need to be addressed.
Atipamezole has not been evaluated as a routine dexmedetomidine reversal agent in cats.
Apnea may occur with Sedaject use. The risk is increased when Sedaject is used in conjunction with ketamine in cats. In the event of apnea, additional oxygen should be supplied. Administration of an atipamezole hydrochloride sterile injection to dogs is warranted when apnea is accompanied by bradycardia and cyanotic mucous membranes.
Anesthetic safety is increased when supplemental oxygen is given by mask or endotracheal tube to cats and dogs anesthetized with intravenous regimes, and this applies to the use of Sedaject as well.
A decrease in body temperature is likely to occur during sedation with Sedaject unless externally maintained. Once established, hypothermia may persist longer than sedation and analgesia. To prevent hypothermia, treated animals should be kept warm and at a constant temperature during the procedure, and until full recovery.
Nervous or excited animals with high levels of endogenous catecholamines may exhibit a reduced pharmacological response to alpha2-adrenoreceptor agonists like dexmedetomidine. In agitated animals, the onset of sedative/analgesic effects could be slowed, or the depth and duration of effects could be diminished or nonexistent. Therefore, allow dogs and cats to rest quietly for 10 to 15 minutes after injection. Repeat dosing has not been evaluated.
Reversible corneal opacity may occur during sedation. An eye lubricant should be applied to prevent corneal desiccation that may result from a reduction in the blink reflex or decrease in tear production during sedation.
Spontaneous muscle contractions (twitching) can be expected in some dogs sedated with Sedaject.
The use of Sedaject as a preanesthetic in dogs and cats significantly reduces the amount of induction and maintenance anesthetic requirements. Careful patient monitoring during anesthetic induction and maintenance is necessary to avoid anesthetic overdose.
Analgesia resulting from preanesthetic Sedaject is dose dependent, and may not provide adequate pain control during the postoperative or postprocedural period. Additional pain management should be addressed as needed.
Administration of anticholinergic agents in dogs at the same time or after Sedaject could lead to adverse cardiovascular effects (secondary tachycardia, prolonged hypertension, and cardiac arrhythmias). However, an anticholinergic drug may be administered at least 10 minutes before Sedaject for the prevention of the Sedaject-induced reduction in heart rate.
Therefore, the routine use of anticholinergics simultaneously with, or after, Sedaject in dogs is not recommended (see ANIMAL SAFETY).
The use of anticholinergics in the presence of dexmedetomidine hydrochloride has not been thoroughly evaluated in cats. Hypertension and a possible increase in myocardial workload may result from concurrent Sedaject and anticholinergic in cats, and the risk/benefit of anticholinergic use should be considered. Routine anticholinergic use is not recommended.
Dexmedetomidine hydrochloride has been evaluated only in fasted dogs; therefore, its effects on fed dogs (for example, the occurrence of vomiting) have not been characterized. In cats, there is a high frequency of vomition whether fed or fasted; therefore, fasting is recommended to reduce stomach contents.
Sedaject has not been evaluated in dogs younger than 16 weeks of age, in cats younger than 12 weeks of age, or in geriatric dogs and cats.
Sedaject has not been evaluated for use in breeding, pregnant, or lactating dogs or cats.
Warnings
Keep out of reach of children.
Dexmedetomidine hydrochloride can be absorbed following direct exposure to skin, eyes, or mouth, and may cause irritation. In case of accidental eye exposure, flush with water for 15 minutes. In case of accidental skin exposure, wash with soap and water. Remove contaminated clothing. Appropriate precautions should be taken while handling and using filled syringes. Accidental topical (including ocular) exposure, oral exposure, or exposure by injection could cause adverse reactions, including sedation, hypotension, and bradycardia. Seek medical attention immediately.
Users with cardiovascular disease (for example, hypertension or ischemic heart disease) should take special precautions to avoid any exposure to this product.
Caution should be exercised when handling sedated animals. Handling or any other sudden stimuli, including noise, may cause a defense reaction in an animal that appears to be heavily sedated.
Adverse Reactions
Although all adverse reactions are not reported, the following information is based on voluntary post-approval drug experience reporting. It is generally recognized this results in significant under-reporting. The adverse events listed here reflect reporting and not necessarily causality. Adverse events are listed by body system, in decreasing order of frequency:
Dogs
Systemic disorders: death, lethargy, anorexia, lack of efficacy, hyperthermia
Cardiovascular system disorders: bradycardia, cardiac arrest, arrhythmia, hypotension
Neurological disorders: convulsion, sedation, muscle tremor
Digestive tract disorders: vomiting, diarrhea, hemorrhagic diarrhea
Respiratory tract disorders: apnea, tachypnea
Cats
Systemic disorders: death, hyperthermia, hypothermia, lethargy, lack of efficacy
Neurological disorders: ataxia, sedation
Respiratory tract disorders: dyspnea, tachypnea, apnea, pulmonary edema
Cardiovascular system disorders: cardiac arrest, bradycardia
Digestive tract disorders: hypersalivation, vomiting
Canine sedation/analgesia field study: In the field study safety analysis, 106 dogs received dexmedetomidine hydrochloride sterile injection and 107 medetomidine hydrochloride sterile injection. Dogs ranged from 16 weeks to 16 years of age, representing 49 breeds. The following table shows the number of dogs displaying each clinical observation (some dogs experienced more than one adverse reaction).
TABLE 4:
Adverse reactions during the canine sedation/analgesia field study:
|
|
Dexmedetomidine HCl |
Medetomidine HCl |
|
Total n = 106 |
Total n = 107 |
|
|
Ausculted unidentified arrhythmias |
19 |
20 |
|
Severe bradycardia requiring treatment |
1 |
1 |
|
Apnea requiring treatment |
1 |
0 |
|
Slow onset of sedation (exceeding 30 minutes) |
1 |
1 |
|
Ineffectiveness (dog standing throughout the study) |
3 |
2 |
|
Severe hypothermia requiring treatment |
2 |
0 |
|
Prolonged recovery |
1 |
4 |
The occurrence of ausculted unidentified arrhythmias (some at multiple time points) decreased following the administration of atipamezole hydrochloride.
Canine preanesthesia field study: The preanesthesia field study safety analysis included 192 dogs, between 5 months and 15 years of age, representing 43 breeds enrolled for elective procedures conducted under general anesthesia. The following table shows the number of dogs within a treatment group that showed each clinical sign (some dogs experienced more than one adverse reaction).
TABLE 5:
Adverse reactions during the canine preanesthesia field study:
|
Treatment Groups |
||||||
|
Induction Anesthetic: |
Propofol |
Barbiturate |
||||
|
Preanesthetic Dose: |
0 µg/m2 n = 32 |
125 µg/m2 n = 32 |
375 µg/m2 n = 32 |
0 µg/m2 n = 32 |
125 µg/m2 n = 32 |
375 µg/m2 n = 32 |
|
Ventricular premature contractions |
0 |
2 |
0 |
4 |
1 |
0 |
|
Severe bradycardia |
0 |
0 |
1 |
0 |
0 |
1 |
|
Tachycardia |
0 |
0 |
0 |
1 |
1 |
0 |
|
Diarrhea |
1 |
0 |
0 |
3 |
1 |
1 |
|
Emesis |
4 |
7 |
4 |
2 |
3 |
6 |
|
Urinary incontinence |
0 |
0 |
0 |
0 |
0 |
1 |
|
Self trauma |
0 |
2 |
1 |
2 |
1 |
0 |
Other clinical signs observed in dogs treated with dexmedetomidine hydrochloride sterile injection include decreased respiratory rate and hypothermia.
Feline sedation/analgesia field study: The field study safety analysis included 242 cats (122 received dexmedetomidine hydrochloride sterile injection; 120 received xylazine), 0.5 to 17 years of age, and representing 19 breeds. The following table shows the number of cats reported with an adverse reaction (some cats experienced more than one adverse reaction).
TABLE 6:
Adverse reactions during the feline field study:
|
|
Dexmedetomidine HCl n = 122 |
Xylazine n = 120 |
|
Vomiting |
70 |
82 |
|
Urinary incontinence |
6 |
11 |
|
Hypersalivation |
4 |
5 |
|
Involuntary defecation |
4 |
1 |
|
Hypothermia |
2 |
1 |
|
Diarrhea |
2 |
0 |
|
Arrhythmia |
1 |
2 |
|
Corneal ulcer |
1 |
0 |
|
Cyanosis |
1 |
0 |
|
Dyspnea |
1 |
0 |
The most frequently observed adverse reaction was vomiting in both fasted and fed cats. Other infrequent clinical signs observed in cats treated with dexmedetomidine hydrochloride sterile injection included fatigue, anorexia, cystitis, and peripheral vascular disorder. One incidence of dyspnea was reported, 43 minutes after dexmedetomidine hydrochloride sterile injection administration during an oral examination/dental procedure. Prior to dexmedetomidine hydrochloride sterile injection, the cat was free of clinical signs, but had a history of asthma and respiratory infection. The cat responded successfully to treatment.
Feline preanesthesia field study: The field study safety analysis included 184 cats (116 received dexmedetomidine; 68 received saline), 0.2 to 16 years of age, and representing 11 breeds. The following table shows the number of cats reported with an adverse reaction (some cats experienced more than one adverse reaction).
TABLE 7:
Adverse reactions during the feline preanesthesia field study:
|
Induction Anesthetic |
Ketamine |
Propofol |
||
|
Preanesthetic |
Saline n = 37 |
Dexmedetomidine HCl n = 64 |
Saline n = 31 |
Dexmedetomidine HCl n = 52 |
|
Apnea |
|
1 |
|
|
|
Behavioural change |
|
|
1 |
|
|
Corneal injury |
1 |
|
|
|
|
Decreased body temperature |
|
4 |
|
|
|
Emesis |
2 |
20 |
1 |
12 |
|
Fluid in endotracheal tube |
|
|
1 |
|
|
Heart murmur |
|
|
|
2 |
|
Loose stool |
|
2 |
|
|
|
Pale mucous membranes |
|
11 |
|
9 |
|
Retching |
|
1 |
1 |
3 |
One case of apnea was reported in a cat that received ketamine as the induction agent. This cat required artificial ventilation from the start of the procedure until 30 minutes into recovery when the cat began to breathe on its own. The cat recovered without further problems.
INFORMATION FOR OWNERS:
Due to the rare possibility of delayed onset of pulmonary edema which has been associated with administration of other alpha2-adrenergic agonists in cats, up to 3 days after use, animal owners should notify their veterinarian immediately if their cat experiences difficulty breathing.
Clinical Pharmacology
Dexmedetomidine is a potent non-narcotic alpha2-adrenoreceptor agonist which produces sedation and analgesia. These effects are dose dependent in depth and duration. Blood pressure is initially increased due to peripheral vasoconstriction, subsequently dropping to normal or slightly below normal levels. Vasoconstriction may cause mucous membranes to appear pale or mildly cyanotic. This initial vasopressor response is accompanied by a compensatory marked decrease in heart rate mediated by a vagal baroreceptor. The peripheral pulse may feel weak and a transient change in the conductivity of the cardiac muscle may occur, as evidenced by first and second degree atrioventricular blocks. Other arrhythmias may occur. Dexmedetomidine also decreases the respiratory rate and decreases body temperature. The magnitude and duration of the decrease in body temperature is dose dependent. Dexmedetomidine causes depression of gastrointestinal motility due to decrease in smooth muscle activity, increases blood glucose levels due to inhibition of insulin release, and increases production of urine. Spontaneous muscle contractions (twitching) can be expected in some dogs sedated with dexmedetomidine. Vomiting in cats has been associated with alpha2-adrenergic agonist central stimulation of the brain.
ANIMAL SAFETY:
Canine safety study: In the multiple dose safety study, dexmedetomidine hydrochloride sterile injection was administered at 0, 1, 3 or 5 times (X) the recommended IV and IM doses on 3 consecutive days to a total of 36 healthy, young beagles. Two additional groups were given a 3X dose of dexmedetomidine hydrochloride sterile injection (IV or IM) followed by three 1X doses of the reversal agent, atipamezole hydrochloride sterile injection, every 30 minutes. This was repeated for a total of 3 days. No deaths occurred during the study.
1X dose group: At the recommended dose, sedation lasted less than 3 hours. During sedation, muscle twitches occurred intermittently, and decreases in temperature, respiratory rate, and heart rate were observed in all animals. A slow pupil response to light was seen transiently about 15 minutes after dosing in one of twelve dogs. Second degree atrioventricular (AV) blocks were observed in one of twelve dogs.
3X dose group: At 3 times the recommended dose, the duration of sedation was between two and eight hours. During sedation, muscle twitches occurred, and temperature, respiratory rate, and heart rate decreased in all dogs. The pupillary light reflex was transiently decreased for up to 90 minutes in four of twelve dogs. Vomiting was seen in two of twelve dogs. One dog experienced first and second degree AV blocks; second degree AV block was observed in three of twelve dogs. Elevated concentrations of alanine aminotransferase (ALT) were observed in one dog, without histological changes to the liver.
5X dose group: At 5 times the recommended dose, the duration of sedation was between four and eight hours. Muscle twitches and decreases in temperature, respiratory rate, and heart rate were seen in all dogs. No pupil response was noted in six of twelve dogs (IV) for up to 1.5 hours; decreased transient pupillary light reflex was seen for up to 60 minutes in two of twelve dogs (IM). Vomiting was seen in one of twelve dogs. First and second degree AV blocks were observed in one of twelve dogs. Elevated concentrations of ALT were observed in 3 of 12 dogs, without histological changes to the liver.
Dexmedetomidine hydrochloride sterile injection demonstrated dose dependent effects related to its pharmacology when administered IV or IM to healthy dogs at doses up to five times the recommended dose.
Canine safety study with an anticholinergic: In another laboratory safety study, one of three doses of an IM anticholinergic drug or saline was administered 10 minutes before, at the same time, or 15 minutes after 500 µg/m2 IM dexmedetomidine hydrochloride sterile injection. The anticholinergic drug was given for the prevention or treatment of dexmedetomidine-induced reduction in heart rate. In a crossover design, 18 dogs were used in a total of 72 trials, to evaluate the safety of dexmedetomidine hydrochloride used with an anticholinergic drug.
Dogs were instrumented for the accumulation of continuous ECG data. The following arrhythmias were recorded during the study (some dogs experienced more than one arrhythmia).
TABLE 8:
Arrhythmias recorded during the canine laboratory safety study:*
|
Type of arrhythmia |
Number of dogs (of 18) |
|
Second degree AV block |
18 |
|
Third degree AV block |
6 |
|
Ventricular escape beats |
16 |
|
Ventricular premature contractions |
14 |
|
Idioventricular rhythm |
1 |
|
Supraventricular tachycardia (SVT) or SVPCs |
16 |
|
Paroxysmal VT |
1 |
|
Ventricular bigeminy; SVPCs; pulse alternans |
1 |
|
Junctional escape beat |
1 |
* Table does not relate arrhythmias to the presence or absence of anticholinergic
The occurrence of arrhythmias was not related to the presence or absence of the anticholinergic drug. Arrhythmias were transient (although frequent over time in some dogs), returning toward baseline levels within 55 minutes after dexmedetomidine hydrochloride sterile injection. No dogs required treatment related to these arrhythmias, and none of these arrhythmias persisted or adversely affected the overall clinical status of any dog in the study.
Dexmedetomidine hydrochloride sterile injection without anticholinergic: Without the anticholinergic drug, and in addition to arrhythmias, dexmedetomidine hydrochloride sterile injection produced clinically relevant sedation accompanied by a statistically significant reduction in heart rate, respiratory rate, cardiac output, pulmonary arterial temperature, and mixed venous oxygen tension. A statistically significant increase in arterial blood pressure, pulmonary capillary wedge pressure, central venous pressure, and systemic vascular resistance was noted. No dogs experienced hypotension. Dexmedetomidine hydrochloride sterile injection tended to increase pulmonary vascular resistance.
Dexmedetomidine hydrochloride sterile injection alone had no statistically significant effect on mean pulmonary arterial pressure, arterial pH, arterial carbon dioxide tension, and arterial oxygen tension.
Dexmedetomidine hydrochloride sterile injection plus anticholinergic: Either of the two higher anticholinergic doses was effective in the prevention or treatment of the dexmedetomidine hydrochloride-induced reduction in heart rate. Anticholinergic (higher doses) given after dexmedetomidine hydrochloride sterile injection caused marked increases in the occurrence of various cardiac arrhythmias, especially second degree AV block. When the higher doses of anticholinergic drug were given at the same time or 15 minutes after dexmedetomidine hydrochloride sterile injection, large increases in heart rate (p<0.01) and blood pressure (p<0.05) were seen. Increases were dose related; the highest anticholinergic dose elicited more frequent arrhythmias and larger increases in heart rate and blood pressure.
In conclusion, moderate doses of anticholinergic drug given prior to dexmedetomidine hydrochloride sterile injection performed best for the prevention of dexmedetomidine hydrochloride-induced reduction of heart rate in dogs.
The routine use of anticholinergics given simultaneously with, or after, Sedaject is not recommended.
Feline safety study: In a multiple dose safety study, dexmedetomidine hydrochloride sterile injection was administered intramuscularly (IM) at 1X, 3X, and 5X (40, 120, and 200 µg/kg) the recommended dose of 40 µg/kg on 3 consecutive days to healthy cats 6 to 8 months old. A control group received the product vehicle as a placebo (0X). No mortality was observed. The depth and duration of sedation was dose dependent, lasting approximately 2 hours in the 1X group, 2 to 4 hours in the 3X group, and greater than 8 hours in the 5X group. The lowest recorded individual heart rate was 60 beats/minute and occurred in the 5X dose group (2 cats). Cardiac arrhythmias characterized by isolated junctional escape complexes with episodes of junctional escape rhythm were observed during periods of low heart rate or following sinus pauses in all dexmedetomidine hydrochloride dose groups. In most cases, the arrhythmia was no longer observed after 1 to 2 hours. Atrioventricular block was not observed. Incidences of arrhythmias were not related to dose; however, more cats were affected by cardiac arrhythmias on the third day of treatment, compared to the first two days of the study. The decrease in respiratory rate, but not the duration, was dose dependent. The rectal temperature decreased in all dexmedetomidine hydrochloride-treated groups, with the lowest temperatures in the 5X group at 8 hours on all three days. Two cats vomited (40 and 120 µg/kg). Corneal opacity was noted in all dexmedetomidine hydrochloride sterile injection-dose groups, was transient, related to dose and duration of sedation, and was attributed to lack of lubrication with decreased blinking during sedation. Hematology and blood chemistry were unaffected by treatment. Injection site tolerance was good, with mild inflammatory lesions representative of the IM injection procedure. Gross and histological examination of all other tissues did not reveal any abnormalities related to dexmedetomidine hydrochloride sterile injection administration.
Dexmedetomidine hydrochloride sterile injection demonstrated dose dependent effects related to its pharmacology when administered IM to healthy cats at doses up to five times the recommended dose.
Feline acute tolerance study: IM dexmedetomidine hydrochloride sterile injection was administered once at 10X (400 µg/kg) the recommended dose of 40 µg/kg to 3 female and 3 male 7 month old cats. No mortality was observed. Sedation was observed within 15 minutes of dosing and lasted for at least 4 hours with full recovery noted between 8 and 24 hours after dosing.
Transient observations of corneal dehydration and opacity, miosis, pale skin and gingiva, salivation, and watery ocular discharge were observed in some animals. Vomiting was observed 7 to 11 hours after dosing in all but one animal. Decreases in heart rate accompanied by prolonged PQ and QT intervals were most pronounced 2 to 4 hours after dosing. No atrioventricular (AV) blocks or escape rhythms were noted. In one cat, incidental and reversible premature junctional complexes were seen at 1 and 2 hours after dosing which were considered secondary to bradycardia. Slightly lower respiratory rate and reduced rectal temperature were observed 4 to 8 hours after dosing.
Observations had returned to normal by 24 hours after dosing. Mild inflammatory lesions observed histologically at the injection site were representative of the IM injection procedure. No treatment related changes were observed in hematology. Mild elevations in some clinical ALT, AST, and CK were observed 24 hours after dosing, with a trend towards recovery by 48 hours. Total protein, albumin and globulin levels were slightly lowered in one cat 48 hours after dosing.
EFFICACY:
Canine sedation/analgesia field study: Dexmedetomidine hydrochloride sterile injection was evaluated in a masked, controlled, multi-site field study, using parallel treatment groups. Effectiveness was evaluated in 200 (of 213) healthy client-owned dogs, ranging in age between 16 weeks and 16 years of age, and in size between 2.2 kg and 64 kg. Dogs admitted to veterinary clinics for various procedures requiring sedation and/or analgesia received either dexmedetomidine hydrochloride sterile injection or medetomidine hydrochloride sterile injection once, by IV or IM injection. Procedures included dental care, radiography, minor skin tumour removal, and treatment of otitis.
Sedation and analgesia occurred within 5 minutes after IV dexmedetomidine hydrochloride sterile injection, and within 15 minutes after IM dexmedetomidine hydrochloride sterile injection, with peak effects approximately at 15 or 30 minutes, respectively. Effects waned by approximately two hours after IV administration, and by three hours using the IM route. Dexmedetomidine hydrochloride sterile injection and medetomidine hydrochloride sterile injection showed comparable clinical effects.
Cardiac rhythms were evaluated by auscultation. Bradycardia occurred within 5 to 15 minutes after IV dexmedetomidine hydrochloride sterile injection or medetomidine hydrochloride sterile injection, and within 15 to 30 minutes after either drug given IM. Sixty-four dexmedetomidine-treated dogs and 50 medetomidine-treated dogs were observed with bradycardia.
Adverse reactions during the field study included ausculted unidentified arrhythmias, apnea, hypothermia, and ineffectiveness (see ADVERSE REACTIONS).
Eleven dogs received concomitant medication during the field study, including amoxicillin, cephalexin, triamcinolone, methyl-prednisolone acetate, neomycin, nystatin, thiostrepton, acepromazine, atropine, and atipamezole.
The results of this field study demonstrate that dexmedetomidine hydrochloride sterile injection produces satisfactory levels of sedation and analgesia for clinical examinations and procedures, minor surgical procedures, and minor dental procedures.
Canine preanesthesia field study: The use of dexmedetomidine hydrochloride sterile injection as a preanesthetic was evaluated in a controlled, multi-site field study, using parallel treatment groups. Effectiveness was evaluated in 192 healthy, client-owned dogs, between 5 months and 15 years of age, weighing 2 kg to 89 kg. Dogs received IM dexmedetomidine hydrochloride sterile injection or saline as a preanesthetic to general anesthesia. All dogs were induced by an injectable anesthetic; half of the dogs were maintained with an inhalation anesthetic. Procedures included castration, ovariohysterectomy, skin surgery, radiography, physical examination, dental procedures, ear cleaning, anal sac treatment, and grooming.
Compared to saline controls, dexmedetomidine hydrochloride sterile injection IM reduced induction drug requirements by 30-36% (at 125 µg/m2) and by 38-61% (at 375 µg/m2). Inhalation anesthetic requirements were 40-60% less for dexmedetomidine hydrochloride sterile injection-preanesthetized dogs. The number of dogs with clinical signs of pain was less for at least 30 minutes after the procedure in dogs treated with 375 µg/m2 dexmedetomidine hydrochloride, compared to saline controls. Recovery times were dose dependent, averaging 15-32 minutes to extubation and 71-131 minutes to standing recovery (longer times correspond to higher dexmedetomidine hydrochloride dose). Recovery times also depended on the induction anesthetic. Recovery times following barbiturate induction were longer (30 minutes to extubation and 118 minutes to standing), compared to dogs induced with propofol (23 minutes to extubation and 84 minutes to standing).
Cardiac arrhythmias were monitored by ECG. Dexmedetomidine hydrochloride sterile injection-treated dogs were more frequently observed with at least one incidence of arrhythmia compared to saline controls. The most commonly observed arrhythmias were bradycardia, 1st and 2nd degree AV block, and sinus arrest. Other less frequently observed arrhythmias included ventricular premature complexes, supraventricular premature complexes, 3rd degree AV block, and sinus pause.
Adverse events included bradycardia, tachycardia, VPCs, vomiting, diarrhea, urinary incontinence, and self trauma (see ADVERSE REACTIONS).
The results of the preanesthesia study demonstrate that dexmedetomidine hydrochloride sterile injection provided anesthetic dose-sparing, sedation, and analgesia during procedures conducted under general anesthesia.
Feline sedation/analgesia field study: Dexmedetomidine hydrochloride sterile injection was evaluated in a masked, controlled, multiple site field study, using parallel treatment groups. Effectiveness was evaluated in 242 client-owned cats, ranging in age between 0.5 and 17 years, and in size between 2.3 and 9.6 kg. Cats admitted to veterinary clinics for various procedures requiring restraint, sedation, and/or analgesia were randomized to treatment group and given dexmedetomidine hydrochloride sterile injection (122 cats) or xylazine (120 cats) once by IM injection. Procedures performed using dexmedetomidine hydrochloride sterile injection included dental care, radiography, minor superficial surgery, otitis treatment, blood or urine sample collection, tattooing, microchip placement, and grooming.
Sedation and analgesia occurred within 5 to 15 minutes and peak effects were observed 30 minutes after dexmedetomidine hydrochloride sterile injection. The procedure was easily performed in 91% of cats beginning 30 minutes after dexmedetomidine hydrochloride sterile injection. Sedative and analgesic effects waned by three hours after dexmedetomidine hydrochloride sterile injection.
Signs of sedation were deeper for cats receiving dexmedetomidine hydrochloride sterile injection compared to those receiving xylazine. No clinically relevant differences were observed between dexmedetomidine hydrochloride sterile injection and xylazine with respect to analgesia or physiological variables. Heart rate, respiratory rate, and rectal temperature decreased. Bradycardia was observed within 5 to 15 minutes and heart rates of ≤70 beats/minute were seen in 18% of cats. The most commonly observed arrhythmias assessed with ECG were atrioventricular dissociation and escape rhythms, followed by a few incidences of premature complexes and one incidence of atrioventricular block. Oxygen saturation, mucous membrane colour, capillary refill time, pulse character, respiratory depth and pattern, and response of the animal to injection were clinically satisfactory. All cats recovered from changes induced by dexmedetomidine hydrochloride sterile injection.
Ninety-seven adverse events were reported after dexmedetomidine hydrochloride sterile injection. The most frequently reported adverse reactions included vomiting (70), urinary incontinence (6), hypersalivation (4), involuntary defecation (4), hypothermia (2), and diarrhea (2) (see ADVERSE REACTIONS).
The results of this field study demonstrate that dexmedetomidine hydrochloride sterile injection produces satisfactory levels of sedation and analgesia for clinical examinations and procedures, minor surgical procedures, and minor dental procedures.
Feline preanesthetic field study: The use of dexmedetomidine hydrochloride sterile injection as a preanesthetic was evaluated in a masked, controlled, multi-site field study, using parallel treatment groups. Effectiveness was evaluated in 182 healthy, client-owned cats, between 12 weeks and 16 years of age, weighing 0.9 kg to 8.5 kg. Premedication-induction drug combinations included saline and ketamine, dexmedetomidine hydrochloride sterile injection and ketamine, saline and propofol and dexmedetomidine hydrochloride sterile injection and propofol. All cats were intubated prior to the procedure. Gas anesthesia (isoflurane) was added during long procedures (>15 minutes) and could be added during a short procedure if the veterinarian deemed it necessary. Procedures that were conducted included (but were not limited to) ovariohysterectomy, orchiectomy, onychectomy, and dental cleaning.
Compared to saline control, dexmedetomidine hydrochloride sterile injection prior to induction with ketamine administered at 5 mg/kg resulted in a significantly higher proportion of cats that were successfully intubated. For the long and short procedures, cats premedicated with saline had intubation success rates of 5.5% and 15.8%, respectively, while cats premedicated with dexmedetomidine hydrochloride sterile injection had intubation success rates of 90.8% and 88.2%, respectively.
Compared to saline control, cats premedicated with dexmedetomidine hydrochloride sterile injection required 48.9% less propofol for successful intubation.
Inhalation anesthetic requirements were 35-44% less for dexmedetomidine hydrochloride sterile injection-preanesthetized cats. The least squares mean visual analog score for pain was less for at least 2 hours after the procedure in cats that received dexmedetomidine hydrochloride sterile injection, compared to saline controls. Recovery times following ketamine and propofol induction averaged 36 and 39 minutes to extubation and 161 and 131 minutes to standing, respectively, for dexmedetomidine hydrochloride sterile injection-treated groups.
Dexmedetomidine hydrochloride sterile injection (followed by ketamine or propofol) resulted in the following ECG abnormalities (in decreasing order of frequency): sinus bradycardia, sinus arrhythmia, 1st degree atrioventricular block, long QT interval, sinus pauses, ventricular premature depolarizations, 2nd degree atrioventricular block, escape beats/rhythms, and supraventricular premature depolarizations. Dexmedetomidine hydrochloride-treated cats had a lower mean heart rate, respiratory rate, and body temperature compared to saline controls. This continued through the recovery period.
Sixty-five adverse events were reported after dexmedetomidine hydrochloride sterile injection. The most frequently reported adverse events were: vomiting (32), pale mucous membranes (20), decreased body temperature (4), and retching (4). (See ADVERSE REACTIONS).
Storage
Store at 15-30°C. Keep from freezing. Discard any remaining product after 28 days.
PRESENTATION:
Sedaject is supplied in 10 mL, multidose vials.
Date of preparation: February, 2022
™Grey Wolf Animal Health Inc.
Grey Wolf Animal Health Inc., 65 Front Street E., Suite 201, Toronto, ON M5E 1B5
1-844-400-GWAH (4924)
CPN: 2022009.1
65 FRONT STREET EAST, SUITE 201, TORONTO, ON, M5E 1B5
| Telephone: | 1-844-400-GWAH | |
| Website: | www.greywolfah.com | |
| Email: | support@greywolfah.com |
 |
THIS SERVICE AND DATA ARE PROVIDED "AS IS". Animalytix assumes no liability, and each user assumes full risk, responsibility, and liability, related to its use of the Animalytix service and data. See the Terms of Use for further details. |

Copyright © 2024 Animalytix LLC. Updated: 2024-02-27
