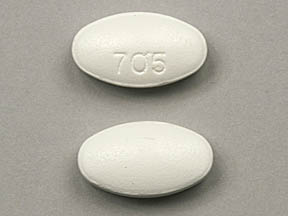
Norfloxacin
Medically reviewed by Drugs.com. Last updated on Aug 2, 2023.
Pronunciation
(nor FLOKS a sin)
Pharmacologic Category
- Antibiotic, Fluoroquinolone
Pharmacology
Norfloxacin is a DNA gyrase inhibitor. DNA gyrase is an essential bacterial enzyme that maintains the superhelical structure of DNA. DNA gyrase is required for DNA replication and transcription, DNA repair, recombination, and transposition; bactericidal
Absorption
Oral: Rapid, up to 40%
Metabolism
Hepatic
Excretion
Urine (26% to 32% as unchanged drug; 5% to 8% as metabolites); feces (30%)
Time to Peak
Serum: 1 to 2 hours
Half-Life Elimination
3 to 4 hours; Renal impairment (CrCl ≤30 mL/minute): 6.5 hours; Elderly: 4 hours
Protein Binding
10% to 15%
Use: Labeled Indications
Uncomplicated and complicated urinary tract infections caused by susceptible gram-negative and gram-positive bacteria; sexually transmitted disease (eg, uncomplicated urethral and cervical gonorrhea) caused by N. gonorrhoeae; prostatitis due to E. coli
Note: As of April 2007, the CDC no longer recommends the use of fluoroquinolones for the treatment of gonococcal disease.
Limitations of use: Because fluoroquinolones have been associated with disabling and potentially irreversible serious adverse reactions (eg, tendinitis and tendon rupture, peripheral neuropathy, CNS effects), reserve norfloxacin for use in patients who have no alternative treatment options for acute uncomplicated urinary tract infections.
Off Label Uses
Infectious Diarrhea
Based on the Infectious Diseases Society of American (IDSA) Practice Guidelines for the Management of Infectious Diarrhea, norfloxacin given for infectious diarrhea is effective and recommended in the management of this condition.
Spontaneous bacterial peritonitis (prevention)
Data from a meta-analysis and controlled trials support the use of norfloxacin as primary long-term prophylaxis in cirrhotic patients with low protein ascites or as secondary long-term prophylaxis in patients who have experienced a prior spontaneous bacterial peritonitis (SBP) episode [Fernández 2007], [Lontos 2014], [Loomba 2009].
Based on American Association for the Study of Liver Diseases guidelines on the management of adult patients with ascites due to cirrhosis and European Association for the Study of the Liver guidelines for the management of patients with decompensated cirrhosis, norfloxacin is recommended for long-term prophylaxis in patients who have experienced a prior SBP episode and for primary prophylaxis in cirrhotic patients with low protein ascites. Norfloxacin can also be used for short-term prophylaxis (7 days) in cirrhotic patients with GI hemorrhage. Increasing bacterial resistance rates to antibiotics used in the treatment and prevention of SBP have been documented; therefore, local epidemiological patterns should be considered, and use of antibiotic prophylaxis should be restricted to patients at high risk of SBP [AASLD [Runyon 2012]], [EASL 2018].
Related/similar drugs
amoxicillin, doxycycline, ciprofloxacin, cephalexin, azithromycin, ceftriaxone, Augmentin
Contraindications
Hypersensitivity to norfloxacin, quinolones, or any component of the formulation; history of tendonitis or tendon rupture associated with quinolone use
Dosing: Adult
Note: Noroxin is no longer available in the US.
Prostatitis: Oral: 400 mg every 12 hours for 4 to 6 weeks
Uncomplicated gonorrhea: Oral: 800 mg as a single dose. Note: As of April 2007, the CDC no longer recommends the use of fluoroquinolones for the treatment of uncomplicated gonococcal disease.
Urinary tract infections: Oral:
Uncomplicated due to E. coli, K. pneumoniae, P. mirabilis: 400 mg twice daily for 3 days
Uncomplicated due to other organisms: 400 mg twice daily for 7 to 10 days
Complicated: 400 mg twice daily for 10 to 21 days
Dysenteric enterocolitis (Shigella) (off-label use): 400 mg twice daily for 3 days (IDSA 2001)
Spontaneous bacterial peritonitis (SBP) (prevention) (off-label use):
Prior SBP or low protein ascites: Long-term prophylaxis: 400 mg once daily (AASLD [Runyon 2012]; EASL 2010)
Variceal hemorrhage: Short-term prophylaxis: 400 mg every 12 hours for 7 days (AASLD [Runyon 2012]; Fernandez 2006). May also administer norfloxacin 400 mg every 12 hours for 7 days after a course of IV ceftriaxone during active GI bleed (AASLD [Runyon 2012]).
Traveler's diarrhea (off-label use): 400 mg twice daily for 3 days (Mattila 1993), single dose may also be effective.
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Refer to adult dosing.
Extemporaneously Prepared
A 20 mg/mL oral suspension may be made using tablets. Crush three 400 mg tablets and reduce to a fine powder. Add a small amount of a 1:1 mixture of Ora-Plus® and Strawberry Syrup (made from a 1:5 mix of Strawberry Fountain Syrup and Simple Syrup, NF) and mix to a uniform paste; mix while adding the vehicle in geometric proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label "shake well". Stable 56 days at room temperature or refrigerated. May administer chocolate syrup before medication administration or mix the suspension 1:1 with chocolate syrup to mask the bitter aftertaste and improve palatability.
Johnson CE, Price J, and Hession JM, "Stability of Norfloxacin in an Extemporaneously Prepared Oral Liquid," Am J Health Syst Pharm, 2001, 58(7):577-9.11296605Administration
Oral: Hold antacids, sucralfate, or multivitamins/supplements containing iron, zinc, magnesium, or aluminum for at least 2 hours before or after giving norfloxacin; do not administer together. Administer on an empty stomach with water (at least 1 hour before or 2 hours after meals, milk, or other dairy products).
Dietary Considerations
Oral formulations should be administered on an empty stomach with water (at least 1 hour before or 2 hours after meals, milk, or other dairy products). Maintain fluid intake to ensure adequate hydration and urinary output.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Keep container tightly closed.
Drug Interactions
Agents with Blood Glucose Lowering Effects: Quinolones may enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Quinolones may diminish the therapeutic effect of Agents with Blood Glucose Lowering Effects. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amphetamines: May enhance the cardiotoxic effect of Quinolones. Monitor therapy
Antacids: May decrease the absorption of Quinolones. Of concern only with oral administration of quinolones. Management: Avoid concurrent administration of quinolones and antacids to minimize the impact of this interaction. Recommendations for optimal dose separation vary by specific quinolone. Consider therapy modification
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Caffeine and Caffeine Containing Products: Norfloxacin may increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Calcium Salts: May decrease the absorption of Quinolones. Of concern only with oral administration of both agents. Management: Consider administering an oral quinolone at least 2 hours before or 6 hours after the dose of an oral calcium supplement to minimize this interaction. Monitor for decrease therapeutic effects of quinolones during coadministration. Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Quinolones. Specifically, the risk of tendonitis and tendon rupture may be increased. Monitor therapy
CycloSPORINE (Systemic): Norfloxacin may decrease the metabolism of CycloSPORINE (Systemic). Monitor therapy
Delamanid: Quinolones may enhance the QTc-prolonging effect of Delamanid. Management: Avoid concomitant use if possible. If coadministration is unavoidable, frequent monitoring of electrocardiograms (ECGs) throughout the full delamanid treatment period should occur. Consider therapy modification
Didanosine: Quinolones may decrease the serum concentration of Didanosine. Didanosine may decrease the serum concentration of Quinolones. Management: Administer oral quinolones at least 2 hours before or 6 hours after didanosine. Monitor for decreased therapeutic effects of quinolones, particularly if doses cannot be separated as recommended. This does not apply to unbuffered enteric coated didanosine. Consider therapy modification
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Heroin: Quinolones may enhance the adverse/toxic effect of Heroin. Monitor therapy
Iron Preparations: May decrease the serum concentration of Quinolones. Management: Give oral quinolones at least several hours before (4 h for moxi- and sparfloxacin, 2 h for others) or after (8 h for moxi-, 6 h for cipro/dela-, 4 h for lome-, 3 h for gemi-, and 2 h for enox-, levo-, nor-, oflox-, peflox, or nalidixic acid) oral iron. Consider therapy modification
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lanthanum: May decrease the serum concentration of Quinolones. Management: Administer oral quinolone antibiotics at least one hour before or four hours after lanthanum. Consider therapy modification
Magnesium Salts: May decrease the serum concentration of Quinolones. Management: Administer oral quinolones several hours before (4 h for moxi/pe/spar/enox-, 2 h for others) or after (8 h for moxi-, 6 h for cipro/dela-, 4 h for lome/pe/enox-, 3 h for gemi-, and 2 h for levo-, nor-, or ofloxacin or nalidixic acid) oral magnesium salts. Consider therapy modification
Methylphenidate: May enhance the cardiotoxic effect of Quinolones. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Quinolones. Specifically, polyvalent cations in multivitamin products may decrease the absorption of orally administered quinolone antibiotics. Management: Administer oral quinolones at least 2 hours before, or 6 hours after, the dose of a multivitamin that contains polyvalent cations (ie, calcium, iron, magnesium, selenium, zinc). Monitor for decreased quinolone efficacy. Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): May decrease the serum concentration of Quinolones. Specifically, minerals in the multivitamin/mineral product may impair absorption of quinolone antibiotics. Management: Administer oral quinolones at least 2 hours before, or 6 hours after, the dose of a multivitamin that contains polyvalent cations (ie, calcium, iron, magnesium, selenium, zinc). Monitor for decreased therapeutic effects of quinolones. Consider therapy modification
Mycophenolate: Quinolones may decrease the serum concentration of Mycophenolate. Specifically, quinolones may decrease concentrations of the active metabolite of mycophenolate. Monitor therapy
Nadifloxacin: May enhance the adverse/toxic effect of Quinolones. Avoid combination
Nitrofurantoin: May diminish the therapeutic effect of Norfloxacin. Avoid combination
Nonsteroidal Anti-Inflammatory Agents: May enhance the neuroexcitatory and/or seizure-potentiating effect of Quinolones. Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Quinolones. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Probenecid: May decrease the excretion of Quinolones. Specifically, probenecid may decreased the renal excretion of quinolone antibiotics. Probenecid may increase the serum concentration of Quinolones. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Sevelamer: May decrease the absorption of Quinolones. Management: Administer oral quinolones at least 2 hours before or 6 hours after sevelamer. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Strontium Ranelate: May decrease the serum concentration of Quinolones. Management: In order to minimize any potential impact of strontium ranelate on quinolone antibiotic concentrations, it is recommended that strontium ranelate treatment be interrupted during quinolone therapy. Avoid combination
Sucralfate: May decrease the serum concentration of Quinolones. Management: Avoid concurrent administration of quinolones and sucralfate to minimize the impact of this interaction. Recommendations for optimal dose separation vary by specific quinolone. Consider therapy modification
Theophylline Derivatives: Quinolones may increase the serum concentration of Theophylline Derivatives. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Avoid use of live attenuated typhoid vaccine (Ty21a) in patients being treated with systemic antibacterial agents. Postpone vaccination until 3 days after cessation of antibiotics and avoid starting antibiotics within 3 days of last vaccine dose. Consider therapy modification
Varenicline: Quinolones may increase the serum concentration of Varenicline. Management: Monitor for increased varenicline adverse effects with concurrent use of levofloxacin or other quinolone antibiotics, particularly in patients with severe renal impairment. International product labeling recommendations vary. Consult appropriate labeling. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Quinolones may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Zinc Salts: May decrease the serum concentration of Quinolones. Management: Give oral quinolones at several hours before (4 h for moxi- and sparfloxacin, 2 h for others) or after (8 h for moxi-, 6 h for cipro/dela-, 4 h for lome-, 3 h for gemi-, and 2 h for enox-, levo-, nor-, pe- or ofloxacin or nalidixic acid) oral zinc salts. Consider therapy modification
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
>1% to 10%:
Central nervous system: Dizziness (2% to 3%), headache (2% to 3%)
Gastrointestinal: Nausea (3% to 4%), abdominal cramping (2%)
Hematologic & oncologic: Eosinophilia (1% to 2%)
Hepatic: Liver enzymes increased (1% to 2%)
≥0.3% to 1%:
Central nervous system: Drowsiness
Dermatologic: Hyperhidrosis, pruritus, rash
Endocrine & metabolic: Decreased WBC count (1%), increased serum alkaline phosphatase (1%)
Gastrointestinal: Abdominal pain, anorectal pain, anorexia, constipation, diarrhea, dyspepsia, flatulence, loose stools, vomiting, xerostomia
Genitourinary: Proteinuria (1%)
Hematologic and oncologic: Decreased platelet count (1%), leukopenia (1%), thrombocytopenia (1%), decreased hematocrit, decreased hemoglobin
Neuromuscular & skeletal: Weakness (1%), back pain
Miscellaneous: Fever
<0.3%, postmarketing, and/or case reports: Abdominal swelling, acute renal failure, agranulocytosis, albuminuria, anaphylactoid reaction, anaphylaxis, angioedema, anxiety, arthralgia, arthritis, ataxia, bitter taste, blurred vision, bursitis, candiduria, casts in urine, chest pain, chills, cholestatic jaundice, Clostridioides (formerly Clostridium) difficile-associated diarrhea, confusion, crystalluria, depression, diplopia, DRESS syndrome, dysgeusia, dysmenorrhea, dyspnea, edema, erythema, erythema multiforme, exacerbation of myasthenia gravis, exfoliative dermatitis, gastrointestinal hemorrhage, glycosuria, Guillain-Barré syndrome, hearing loss, heartburn, hematuria, hemolytic anemia (sometimes associated with G6PD deficiency), hepatic failure, hepatic necrosis, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani 2014), hypercholesterolemia, hyperglycemia, hyperkalemia, hypersensitivity angiitis, hypersensitivity reaction, hypertriglyceridemia, hypoesthesia, hypoglycemia, increased blood urea nitrogen, increased creatine phosphokinase, increased intracranial pressure, increased lactate dehydrogenase, increased serum creatinine, insomnia, interstitial nephritis, jaundice, muscle spasm, myalgia, myocardial infarction, myoclonus, neutropenia, nystagmus, oral mucosa ulcer, orthostatic hypotension, palpitations, pancreatitis (rare), paresthesia, peripheral edema, peripheral neuropathy (may be irreversible), phototoxicity, prolonged prothrombin time, prolonged QT interval on ECG, pruritus ani, pseudotumor cerebri, psychotic reaction, renal colic, rupture of tendon, seizure, skin photosensitivity, Stevens-Johnson syndrome, stomatitis, tendonitis, tingling of the fingers, tinnitus, torsades de pointes, toxic epidermal necrolysis, tremor, urticaria, uveitis, vasculitis, ventricular arrhythmia, vulvovaginal candidiasis
ALERT: U.S. Boxed Warning
Serious adverse reactions:Fluoroquinolones are associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects. Discontinue norfloxacin immediately and avoid the use of fluoroquinolones in patients who experience any of these serious adverse reactions. Because fluoroquinolones are associated with serious adverse reactions, reserve norfloxacin for use in patients who have no alternative treatment options for uncomplicated urinary tract infections (including cystitis).
Exacerbation of myasthenia gravis:Fluoroquinolonesmay exacerbate muscle weakness in patients with myasthenia gravis. Avoid norfloxacin in patients with known history of myasthenia gravis.
Warnings/Precautions
Concerns related to adverse effects:
• Altered cardiac conduction: Fluoroquinolones may prolong QTc interval; avoid use in patients with a history of QTc prolongation, uncorrected hypokalemia, hypomagnesemia, or concurrent administration of other medications known to prolong the QT interval (including Class Ia and Class III antiarrhythmics, cisapride, erythromycin, antipsychotics, and tricyclic antidepressants).
• Aortic aneurysm and dissection: Fluoroquinolones have been associated with aortic aneurysm ruptures or dissection within 2 months following use, particularly in elderly patients. Fluoroquinolones should not be used in patients with a known history of aortic aneurysm or those at increased risk, including patients with peripheral atherosclerotic vascular diseases, hypertension, genetic disorders involving blood vessel changes (eg, Marfan syndrome, Ehlers-Danlos syndrome), and elderly patients, unless no other treatment options are available. Longer treatment duration (eg, >14 days) may increase risk (Lee 2018).
• Glucose regulation: Fluoroquinolones have been associated with the development of serious, and sometimes fatal, hypoglycemia. These events have occurred most often in elderly patients with diabetes, but have also been reported in patients without a prior history of diabetes. Prompt identification and treatment of hypoglycemia is essential. Individual quinolones may differ in their potential to cause this effect. It was most evident with gatifloxacin (no longer marketed as s systemic formulation). Hyperglycemia has also been associated with the use of fluoroquinolones. Patients should be monitored closely for signs/symptoms of disordered glucose regulation.
• Hypersensitivity reactions: Severe hypersensitivity reactions, including anaphylaxis, have occurred with quinolone therapy. The spectrum of these reactions can vary widely; reactions may present as typical allergic symptoms (eg, itching, urticaria, rash, edema) after a single dose, or may manifest as severe idiosyncratic dermatologic (eg, Stevens-Johnson, toxic epidermal necrolysis), vascular (eg, vasculitis), pulmonary (eg, pneumonitis), renal (eg, nephritis), hepatic (eg, hepatic failure or necrosis), and/or hematologic (eg, anemia, cytopenias) events, usually after multiple doses. Prompt discontinuation of drug should occur if skin rash or other symptoms arise.
• Phototoxicity: Avoid excessive sunlight and take precautions to limit exposure (eg, loose fitting clothing, sunscreen); may cause moderate-to-severe phototoxicity reactions. Discontinue use if photosensitivity occurs.
• Serious adverse reactions: [US Boxed Warning]: Fluoroquinolones are associated with disabling and potentially irreversible serious adverse reactions that may occur together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects. Discontinue norfloxacin immediately and avoid use of fluoroquinolones in patients who experience any of these serious adverse reactions. Patients of any age or without pre-existing risk factors have experienced these reactions; may occur within hours to weeks after initiation.
- CNS effects: Fluoroquinolones have been associated with an increased risk of CNS effects including seizures, increased intracranial pressure (including pseudotumor cerebri), and toxic psychosis; may also cause nervousness, agitation, insomnia, anxiety, nightmares, paranoia, dizziness, confusion, tremors, hallucinations, depression, and suicidal thoughts or actions. May occur following the first dose; discontinue immediately and avoid further use of fluoroquinolones in patients who experience these reactions. Use with caution in patients with known or suspected CNS disorder, or risk factors that may predispose to seizures or lower the seizure threshold.
- Peripheral neuropathy: Fluoroquinolones have been associated with an increased risk of peripheral neuropathy; may occur soon after initiation of therapy and may be irreversible; discontinue if symptoms of sensory or sensorimotor neuropathy occur. Avoid use in patients who have previously experienced peripheral neuropathy.
- Tendinitis/tendon rupture: Fluoroquinolones have been associated with an increased risk of tendonitis and tendon rupture in all ages; risk may be increased with concurrent corticosteroids, solid organ transplant recipients, and in patients >60 years of age, but has also occurred in patients without these risk factors. Rupture of the Achilles tendon has been reported most frequently; but other tendon sites (eg, rotator cuff, biceps, hand) have also been reported. Inflammation and rupture may occur bilaterally. Cases have been reported within hours or days of initiation, and up to several months after discontinuation of therapy. Strenuous physical activity, renal failure, and previous tendon disorders may be independent risk factor for tendon rupture. Discontinue at first sign of tendon pain, swelling, inflammation or rupture. Avoid use in patients with a history of tendon disorders or who have experienced tendinitis or tendon rupture.
• Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
• Myasthenia gravis: [US Boxed Warning]: May exacerbate muscle weakness related to myasthenia gravis; avoid use in patients with known history of myasthenia gravis. Cases of severe exacerbations, including the need for ventilatory support and deaths have been reported.
• Renal impairment: Use caution with renal impairment; dose adjustment required. May increase risk of tendon rupture.
• Rheumatoid arthritis: Use with caution in patients with rheumatoid arthritis; may increase risk of tendon rupture.
• Syphilis: Since norfloxacin is ineffective in the treatment of syphilis and may mask symptoms, all patients should be tested for syphilis at the time of gonorrheal diagnosis and 3 months later.
Special populations:
• Elderly: Adverse effects (eg, tendon rupture, QT changes) may be increased in the elderly.
• G6PD deficiency: Hemolytic reactions may (rarely) occur with fluoroquinolone use in patients with G6PD deficiency (Luzzatto 2020).
• Pediatric: Safety and efficacy have not been established in children; other quinolones have caused transient arthropathy in children.
Other warnings/precautions:
• Appropriate use: [US Boxed Warning]: Reserve use of norfloxacin for treatment of uncomplicated urinary tract infections, including cystitis, for patients who have no alternative treatment options because of the risk of disabling and potentially serious adverse reactions (eg, tendinitis and tendon rupture, peripheral neuropathy, CNS effects).
Monitoring Parameters
Monitor CBC, renal and hepatic function periodically if therapy is prolonged.
Pregnancy Risk Factor C Pregnancy Considerations
Adverse events have been observed in some animal reproduction studies. Norfloxacin crosses the placenta, distributing to cord blood and amniotic fluid (Wise 1984). Based on available data, an increased risk of teratogenic effects has not been observed following norfloxacin use during pregnancy (Bar-Oz 2009; Padberg 2014).
Patient Education
What is this drug used for?
• It is used to treat bacterial infections.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Nausea
• Vomiting
• Lack of appetite
• Fatigue
• Constipation
• Diarrhea
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
• Tendon inflammation or rupture like pain, bruising, or swelling in the back of the ankle, shoulder, hand, or other joints
• Depression like thoughts of suicide, anxiety, emotional instability, or confusion
• Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
• Nerve problems like sensitivity to heat or cold; decreased sense of touch; burning, numbness, or tingling; pain, or weakness in the arms, hands, legs, or feet
• High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
• Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
• Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating
• Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
• Chest pain
• Fast heartbeat
• Abnormal heartbeat
• Dizziness
• Passing out
• Severe loss of strength and energy
• Sensing things that seem real but are not
• Agitation
• Restlessness
• Anxiety
• Nightmares
• Trouble sleeping
• Seizures
• Vision changes
• Confusion
• Behavioral changes
• Severe headache
• Shortness of breath
• Bruising
• Bleeding
• Purple spots or redness of skin
• Chills
• Noise or ringing in the ears
• Tremors
• Abnormal gait
• Muscle pain
• Vaginal pain, itching, and discharge
• Thrush
• Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
More about norfloxacin
- Check interactions
- Compare alternatives
- Reviews (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Patient resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.