Monomethyl Fumarate
Medically reviewed by Drugs.com. Last updated on Sep 21, 2023.
Pronunciation
(MON oh METH il FUE ma rate)
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
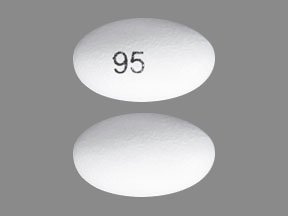
Capsule Delayed Release, Oral, as fumarate:
Bafiertam: 95 mg [contains cremophor rh40]
Brand Names: U.S.
- Bafiertam
Pharmacologic Category
- Fumaric Acid Derivative
Pharmacology
Monomethyl fumarate (MMF) and its prodrug, dimethyl fumarate, have been shown to activate the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) pathway, which is involved in cellular response to oxidative stress. The mechanism by which monomethyl fumarate exerts a therapeutic effect in multiple sclerosis is unknown, although it is believed to result from its anti-inflammatory and cytoprotective properties via activation of the Nrf2 pathway (Fox 2012; Gold 2012). MMF has also been identified as a nicotinic acid receptor agonist in vitro.
Absorption
High-fat, high-calorie meals prolong absorption and decrease Cmax by 20%.
Distribution
Vd (prodrug dimethyl fumarate): 53 to 73 L.
Metabolism
Through the tricarboxylic acid cycle, with no involvement of the CYP-450 system.
Excretion
From studies with dimethyl fumarate: Exhalation of CO2: ~60% of dimethyl fumarate; urine (16% of dimethyl fumarate; trace amounts as unchanged monomethyl fumarate); feces (1% of dimethyl fumarate).
Time to Peak
4.03 hours; after high-fat meal: 11 hours.
Half-Life Elimination
~0.5 hour.
Protein Binding
Prodrug dimethyl fumarate: 27% to 45%.
Use: Labeled Indications
Multiple sclerosis, relapsing: Treatment of relapsing forms of multiple sclerosis, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Contraindications
Hypersensitivity (eg, anaphylaxis, angioedema) to monomethyl fumarate, dimethyl fumarate, diroximel fumarate, or to any component of the formulation; concomitant use with dimethyl fumarate or diroximel fumarate.
Dosing: Adult
Multiple sclerosis, relapsing: Oral: Initial: 95 mg twice daily; after 7 days, increase to the maintenance dose: 190 mg twice daily.
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Intolerance to the maintenance dose: Consider temporary dose reduction to 95 mg twice daily; resume recommended maintenance dose of 190 mg twice daily within 4 weeks. Consider discontinuation in patients who cannot tolerate return to the maintenance dose.
Administration
Oral: Swallow capsules whole and intact; do not crush, chew, or mix the contents with food. Administer with or without food. Administration of non–enteric-coated aspirin up to a dose of 325 mg 30 minutes prior to monomethyl fumarate may reduce the incidence of flushing.
Storage
Store unopened bottles in refrigerator at 2°C to 8°C (35°F to 46°F). Do not freeze.
Store opened bottles at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F). Protect from light. Store in original container. Under these conditions, monomethyl fumarate is stable for 3 months.
Drug Interactions
Dimethyl Fumarate: Monomethyl Fumarate may enhance the adverse/toxic effect of Dimethyl Fumarate. Avoid combination
Diroximel Fumarate: Monomethyl Fumarate may enhance the adverse/toxic effect of Diroximel Fumarate. Avoid combination
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
All adverse reactions are reported with dimethyl fumarate, the prodrug of monomethyl fumarate.
>10%:
Cardiovascular: Flushing (40%)
Gastrointestinal: Abdominal pain (18%), diarrhea (14%), nausea (12%)
Infection: Infection (60%)
1% to 10%:
Dermatologic: Erythema of skin (5%) pruritus (8%), skin rash (8%)
Endocrine & metabolic: Albuminuria (6%)
Gastrointestinal: Dyspepsia (5%), vomiting (9%)
Hematologic & oncologic: Lymphocytopenia (2% to 6%)
Hepatic: Increased serum aspartate aminotransferase (4%)
<1%: Nervous system: Progressive multifocal leukoencephalopathy
Frequency not defined:
Hematologic & oncologic: Eosinophilia
Hepatic: Increased liver enzymes, increased serum alanine aminotransferase
Hypersensitivity: Anaphylaxis, angioedema
Postmarketing:
Hepatic: Abnormal liver function, increased serum bilirubin, increased serum transaminases
Infection: Aspergillosis, cytomegalovirus disease, herpes simplex infection, herpes zoster infection (including disseminated, ophthalmicus, meningoencephalitis, and meningomyelitis), listeriosis, opportunistic infection, tuberculosis
Warnings/Precautions
Concerns related to adverse effects:
• Flushing: May cause mild to moderate flushing (eg, warmth, redness, itching, burning sensation); flushing generally appears soon after initiation, and improves or resolves with subsequent dosing. Administration of aspirin (non–enteric coated ≤325 mg) 30 minutes prior to monomethyl fumarate or a temporary dose reduction may also reduce the incidence and severity of flushing.
• Hepatotoxicity: Clinically significant postmarketing cases of hepatic injury have been reported with the prodrug dimethyl fumarate, with an onset ranging from a few days to several months after treatment initiation. Signs/symptoms of hepatic injury, including transaminase elevations >5 times the ULN and total bilirubin elevations >2 times ULN have been observed. Some cases have required hospitalization; however, none of the cases were fatal or resulted in liver failure or transplant. LFT abnormalities resolved upon discontinuation. Drug-induced hepatocellular injury resulting in new-onset transaminase elevations combined with increased bilirubin levels is an important predictor of serious hepatic injury that may lead to acute hepatic failure, liver transplant, or death in some patients. Transaminase elevations (usually <3 times ULN) were observed in clinical trials with dimethyl fumarate; transaminase elevations ≥3 times ULN occurred rarely. Monitor LFTs prior to treatment initiation and during treatment. Discontinue treatment if monomethyl fumarate–induced hepatic injury is suspected.
• Hypersensitivity reactions: Anaphylaxis and angioedema may occur after the first dose or at any time during treatment. Discontinue therapy if signs and symptoms of anaphylaxis or angioedema occur.
• Infections: Serious cases of herpes zoster (eg, disseminated, ophthalmicus, meningoencephalitis, meningomyelitis) have been reported with the prodrug dimethyl fumarate; may develop any time during treatment. Other serious opportunistic infections have occurred, including viral (eg, Cytomegalovirus, herpes simplex, West Nile), fungal (eg, Aspergillus, Candida), and bacterial (eg, Listeria monocytogenes, Mycobacterium tuberculosis, Nocardia), in patients with and without lymphopenia. Consider temporary interruption of therapy until infection has resolved.
• Lymphopenia: Decreased lymphocyte counts may occur. The risk for lymphopenia is not reduced over time with dimethyl fumarate, the prodrug of monomethyl fumarate. A decline in absolute lymphocyte count (ALC) typically occurs in the first year of treatment and stabilizes. Obtain a CBC including lymphocyte count prior to initiation of therapy, then 6 months after initiation, then every 6 to 12 months thereafter, or as clinically indicated. Monitor for signs of infection in patients with lower lymphocyte counts at baseline and mild to moderate lymphopenia (Baharnoori 2018). Consider therapy interruption in patients with lymphocyte counts <500/mm3 persisting >6 months and in patients with serious infections. Progressive multifocal leukoencephalopathy (PML) may occur in patients with a lymphocyte count <500/mm3 for <6 months (Lehmann-Horn 2016). Due to a potential for delayed lymphocyte recovery following treatment interruption or discontinuation, monitor lymphocyte counts until lymphopenia is resolved. The decision to restart monomethyl fumarate should be individualized based on clinical circumstances. Neither monomethyl fumarate nor dimethyl fumarate have been studied in patients with preexisting low lymphocyte counts.
• Progressive multifocal leukoencephalopathy: Cases of PML due to the John Cunningham (JC) virus, including fatality, have been reported with the prodrug dimethyl fumarate. Risk factors for development of PML include HIV, AIDS, cancer history, persistent leukocytopenia, sarcoidosis, and prior immunosuppressant use (Jamilloux 2014; Tan 2010). However, cases have been reported with dimethyl fumarate use in patients who were not immunocompromised and had no prior exposure to immunosuppressive drugs, including natalizumab. Severe, long-standing lymphopenia was identified as a primary risk for PML, and the majority of PML cases occurred in patients with lymphocyte counts <800/mm3 persisting for >6 months (although the exact role of lymphopenia in PML is unknown). At the first sign or symptom suggestive of PML, withhold therapy immediately and perform a diagnostic evaluation; symptoms progress over days to weeks and may include progressive weakness on one side of the body or clumsiness of limbs, vision disturbances, and mental status changes. Cases of PML have been diagnosed based on MRI findings and the detection of JC virus DNA in the cerebrospinal fluid without specific PML signs/symptoms. Monitoring with brain MRI for signs that may be consistent with PML may be beneficial and allow for an early diagnosis of PML (EMA 2015).
Monitoring Parameters
CBC including lymphocyte counts (prior to initiation of therapy, 6 months after initiation, then every 6 to 12 months thereafter as clinically necessary); LFTs including transaminases, alkaline phosphatase, and total bilirubin (prior to treatment initiation and during treatment as clinically indicated); MRI (baseline and as clinically indicated to monitor for early signs of progressive multifocal leukoencephalopathy).
Reproductive Considerations
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy except in females at high risk of MS activity (AAN [Rae-Grant 2018]). Consider use of agents other than monomethylfumarate for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]).
Pregnancy Considerations
In general, disease-modifying therapies for multiple sclerosis (MS) are not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). When disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/ EAN [Montalban 2018]).
Patient Education
What is this drug used for?
• It is used to treat MS (multiple sclerosis).
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Flushing
• Abdominal pain
• Diarrhea
• Nausea
• Vomiting
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Progressive multifocal leukoencephalopathy like confusion, depression, trouble remembering things, behavioral changes, change in strength on one side is greater than the other, trouble speaking, change in balance, or vision changes
• Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
• Sore throat
• Infection
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Frequently asked questions
More about monomethyl fumarate
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: selective immunosuppressants
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.