Goserelin (Monograph)
Brand name: Zoladex
Drug class: Gonadotropins
VA class: AN500
Chemical name: 2-(Aminocarbonyl)hydrazide-6-[O-(1,1-dimethylethyl)-d-serine]-10-deglycinamide luteinizing hormone-releasing factor (pig)
Molecular formula: C59H84N18O14
CAS number: 65807-02-5
Introduction
Synthetic analog of gonadotropin-releasing hormone (GnRH, luteinizing hormone-releasing hormone, gonadorelin); used as an antineoplastic agent and for its endocrine effects.1 2
Uses for Goserelin
Prostate Cancer
Palliative treatment of advanced prostate cancer.1 2 4 5 6 9 10 17 18 Considered one of several first-line options for hormonal therapy; other options include orchiectomy, estrogens, and antiandrogens.9
In clinical studies, goserelin (3.6 mg every 4 weeks) was as effective as orchiectomy.1 2 4 5 17 18 Clinical outcome in patients receiving goserelin 10.8 mg every 12 weeks expected to be similar to that of patients receiving goserelin 3.6 mg every 4 weeks.2 6
Also used as an adjunct to radiation therapy in patients with stage III [C]) prostate cancer.8 10
Treatment of locally confined stage T2b-T4 (B2-C) prostate cancer in conjunction with flutamide and radiation therapy.1 2 20
Endometriosis
Palliative treatment of endometriosis.1 3 5 11 12 Experience with goserelin has been limited to women ≥18 years of age who received consecutive therapy (3.6 mg every 4 weeks) for 6 months.1
Breast Cancer
Palliative treatment of advanced breast cancer in premenopausal and perimenopausal women.1 5 13 15
Use of ovarian suppression in combination with endocrine therapy (i.e., anastrozole, exemestane, letrozole, tamoxifen)† [off-label] as adjuvant therapy† [off-label] in premenopausal women with early-stage hormone receptor-positive breast cancer† [off-label] may be considered a reasonable choice (accepted).10010 10011 10012 10013 10023 10026 10028
Dysfunctional Uterine Bleeding
Used as an endometrial-thinning agent prior to endometrial ablation procedures for the treatment of dysfunctional uterine bleeding.1 3 16
Related/similar drugs
estradiol, tamoxifen, testosterone, norethindrone, Premarin, tranexamic acid, medroxyprogesterone
Goserelin Dosage and Administration
General
Determine serum testosterone concentrations periodically in patients with prostate cancer in whom the anticipated clinical or biochemical response to goserelin has not been achieved.2
Reduction in serum prostate specific antigen (PSA) concentrations may provide information about duration of progression-free status in men with prostate cancer.9 Do not rely solely on PSA concentrations to monitor response because decreases in PSA concentration may occur independent of tumor response.9
Sub-Q
Administered as a biodegradable implant into the anterior abdominal wall below the navel line.1 2 3 4
Implants containing goserelin 3.6 mg are administered every 4 weeks.1 2 3 4
Implants containing goserelin 10.8 mg are administered every 12 weeks.2 6
Adherence to the recommended schedule recommended; a delay of a few days is permitted.1 2
The implant may be located by ultrasound in the event that it needs to be removed.1 2
Consult the manufacturer’s labeling for proper methods of administration and associated precautions.1 2
Dosage
Available as goserelin acetate; dosage expressed in terms of goserelin.1 2
Adults
Prostate Cancer
Advanced Prostate Cancer
Sub-QOne implant containing 3.6 mg every 4 weeks or one implant containing 10.8 mg every 12 weeks.1 2 4 6 Intended for long-term administration 1 2 8 unless it is clinically inappropriate.1 2
Stage III [C]) prostate cancer (as an adjunct to radiation therapy): One implant containing 3.6 mg every 4 weeks; initiate therapy on the first day of radiation or during the last week of radiation.8 10
Stage B2-C Prostate Cancer
Sub-QOne implant containing 3.6 mg every 4 weeks starting 8 weeks prior to radiation therapy and continuing for a total of 4 doses recommended by the manufacturer.1 2 7 Alternatively, one implant containing 3.6 mg implanted 8 weeks prior to radiation therapy and followed by one implant containing 10.8 mg on day 28 (4 weeks after initial 3.6-mg dose) recommended by the manufacturer.1 2
Endometriosis
Sub-Q
One implant containing 3.6 mg every 4 weeks for 6 consecutive months.1 3 11 12 Retreatment with additional courses currently not recommended; safety has only been established for a 6-month course of therapy; there are concerns about potential long-term effects on bone density.1 Assess bone density if retreatment for recurrence is considered.1 (See Musculoskeletal Effects under Cautions.)
Breast Cancer
Advanced Breast Cancer
Sub-QOne implant containing 3.6 mg every 4 weeks.1 13 Consider dosage increase to 7.2 mg (3.6 mg implanted to 2 different sites) every 4 weeks in women whose serum estradiol concentrations are not reduced to postmenopausal levels after 8 weeks.1 13 Intended for long-term administration unless clinically inappropriate.1 2
Early-stage† [off-label] Breast Cancer
Sub-QDosage of one implant containing 3.6 mg every 4 weeks has been used in combination with endocrine therapy† [off-label].10013 10023 (See Breast Cancer under Uses.)
Dysfunctional Uterine Bleeding
Sub-Q
One implant containing 3.6 mg 4 weeks before endometrial ablation.1 Alternatively, the initial 3.6-mg dose of goserelin can be followed by a second 3.6-mg dose 4 weeks after the first dose; surgery should be performed 2–4 weeks after the second dose.1
Prescribing Limits
Adults
Endometriosis
Sub-Q
Maximum 3.6 mg every 4 weeks for 6 consecutive months.1
Special Populations
Hepatic Impairment
Dosage adjustment not needed in patients with mild to moderate hepatic impairment.1 2 Not studied in patients with severe hepatic insufficiency.1 2
Renal Impairment
Dosage adjustment not needed.1 2 (See Special Populations under Pharmacokinetics.)
Geriatric Patients
Dosage adjustment not needed.1 2
Cautions for Goserelin
Contraindications
-
Known hypersensitivity to goserelin or any ingredient in the formulation, other GnRH agonists, or GnRH.1 2
-
Known or suspected pregnancy unless being used for palliative treatment of advanced breast cancer.1
-
Abnormal vaginal bleeding of unknown etiology.1
-
The implant containing 10.8 mg of goserelin should not be used in women; insufficient data available to determine whether this preparation is associated with reliable suppression of serum estradiol.2
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Antibody formation and acute anaphylactic reactions reported with GnRH agonists, including goserelin.1 2
Fetal/Neonatal Morbidity and Mortality
Expected hormonal changes increase the risk for pregnancy loss and fetal harm when administered to a pregnant woman; increased risk of pregnancy loss demonstrated in animals.1 2
Women of childbearing potential should avoid pregnancy and use an effective nonhormonal method of contraception during therapy and for 12 weeks following the last dose of goserelin.1 21 Continuous use of goserelin usually inhibits ovulation and stops menstruation; however, prevention of pregnancy is not ensured.1
Exclude pregnancy before initiating therapy in women with benign gynecologic conditions.1 If a patient with endometriosis or undergoing endometrial thinning becomes pregnant during therapy, discontinue the drug and advise patient about potential fetal hazard.1 2
If used during pregnancy in women with advanced breast cancer, apprise of potential fetal hazard.1
Endocrine Effects
Possible worsening of signs and/or symptoms of prostate or breast cancer (e.g., increased bone pain) and/or development of new manifestations due to transient increases in serum testosterone (in men) or estrogen (in women) concentrations during the initial weeks of therapy.1 2 Concomitant therapy with an antiandrogen (e.g., bicalutamide, flutamide, nilutamide) 1 week before and during the first few weeks of goserelin therapy may minimize disease flare in men with prostate cancer.4 9
Spinal cord compression and/or ureteral obstruction reported in men with prostate cancer.1 2 If spinal cord compression or renal impairment secondary to ureteral obstruction develops, institute standard treatment of these complications; consider immediate orchiectomy in extreme cases.1 2 Caution in patients at particular risk of developing spinal cord compression or ureteral obstruction; observe closely during the first month of therapy.1 2 4 Treat spinal cord compression or ureteral obstruction before initiating goserelin.1 2 4
Possible hyperglycemia and increased risk of diabetes in patients receiving GnRH agonists for treatment of prostate cancer.1 2 23 Studies evaluating risk of diabetes in women and children receiving GnRH agonists not performed to date.22 Evaluate patients for risk factors for diabetes and carefully weigh benefits and risks of GnRH agonist therapy before selecting treatment for prostate cancer.23 Periodically monitor blood glucose and/or HbA1c in patients receiving GnRH agonists for treatment of prostate cancer.1 2 23 Manage hyperglycemia or diabetes according to current standards of care.1 2
Possible increase in cervical resistance.1 Perform cervical dilation carefully following use of goserelin as an endometrial thinning agent.1
Cardiovascular Effects
Possible increased risk of cardiovascular disease (e.g., MI, sudden cardiac death, stroke) in patients receiving GnRH agonists for treatment of prostate cancer.1 2 23 Studies evaluating risk of cardiovascular disease in women and children receiving GnRH agonists not performed to date.22
Evaluate patients for cardiovascular risk factors and carefully weigh benefits and risks of GnRH agonist therapy before selecting treatment for prostate cancer.1 2 23
Periodically monitor patients receiving GnRH agonists for manifestations of cardiovascular disease; manage cardiovascular disease according to current standards of care.1 2 23
Cases of serious venous and arterial thromboembolism (e.g., DVT, PE, MI, TIA, stroke) reported in women receiving GnRH agonists.1
Possible transient changes in BP (hypotension or hypertension).1
Possible increased total cholesterol, LDL cholesterol, and triglycerides and decreased HDL cholesterol.1
Musculoskeletal Effects
Decreases in bone mineral density (BMD), osteoporosis, and bone fracture reported in men; decreases in BMD reported in women.1 2 Currently available data suggest that recovery of bone loss occurs following cessation of therapy most women.1
For management of endometriosis in women, concurrent use of hormone replacement therapy or bisphosphonates (e.g., alendronate) may minimize bone mineral loss associated with GnRH agonist therapy without compromising efficacy.1 19
For treatment of prostate cancer in men, concurrent use of bisphosphonates may minimize bone mineral loss associated with GnRH agonist therapy.1 2
Risk of BMD loss may be increased in patients with a history of prior therapy that resulted in BMD loss and/or patients with risk factors for decreased BMD (e.g., chronic alcohol abuse, tobacco abuse, family history of osteoporosis, chronic use of anticonvulsants or corticosteroids).1
Hypercalcemia reported in patients with prostate or breast cancer with bone metastases.1 2 Initiate appropriate treatment if hypercalcemia develops.1
Prolongation of QT Interval
Possible QT-interval prolonlgation.1 2 Consider monitoring ECG and serum electrolyte concentrations periodically during therapy.1 2 Correct electrolyte abnormalities.1 2
Weigh benefits and risks of androgen deprivation therapy in patients with congenital long QT syndrome, electrolyte abnormalities, or CHF and in patients taking drugs known to prolong the QT interval.1 2
Local Reactions
Injection site injury and vascular injury (e.g., pain, hematoma, hemorrhage, hemorrhagic shock) requiring blood transfusion and surgical intervention reported.1 2
Administer with caution in patients with low BMI and/or those receiving full-dose anticoagulation therapy.1 2
Pituitary Apoplexy
Pituitary apoplexy, a clinical syndrome resulting from infarction of the pituitary gland, and pituitary adenoma reported rarely.1 2 Most cases occur within 2 weeks of the first dose, sometimes within the first hour.1 2 If manifestations occur (e.g., sudden headache, vomiting, visual changes, ophthalmoplegia, altered mental status, sometimes cardiovascular collapse), immediate medical attention required.1 2
Specific Populations
Pregnancy
May cause fetal harm.1 2 (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Distributed into milk in rats; not known whether distributed into human milk.1 Discontinue nursing or the drug.1 2
Pediatric Use
Safety and efficacy not established.1 2
Geriatric Use
Clinical studies for use in prostate cancer have been conducted principally in patients ≥65 years of age.1 2 4 5 6 7 8 21 Clinical studies in women >65 years of age not performed to date.1
Renal Impairment
Incidence of adverse effects not increased in patients with renal impairment receiving goserelin 10.8 mg.2
Common Adverse Effects
Men: Hot flushes (flashes), sexual dysfunction, decreased erections, lower urinary tract symptoms, pain (worsened in the first month).1 2 4 17
Women: Hot flushes (flashes), vaginitis, headache, emotional lability, decreased/increased libido, sweating, depression, acne, breast atrophy, breast enlargement.1 3
Drug Interactions
No formal drug interaction studies to date.1 2
Goserelin Pharmacokinetics
Absorption
Bioavailability
Well absorbed following sub-Q administration.1 2
3.6 mg: Peak plasma concentrations achieved within 12–15 days in men and 8–22 days in women.1 2
10.8 mg: Peak plasma concentrations achieved within 24 hours in men.1 2
Duration
Special Populations
Long-term administration of goserelin 10.8 mg in patients with renal impairment not associated with accumulation of goserelin.2
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.1 Crosses the placenta in rats and rabbits.1
Plasma Protein Binding
Elimination
Metabolism
Undergoes hydrolysis of the C-terminal amino acids.1 2
Elimination Route
Eliminated predominately in urine (90%) as metabolites and unchanged drug (20%).1 2
Half-life
Special Populations
Men with Clcr <20 mL/minute: Half-life of 12.1 hours reported.1 2
Similar total body clearance and elimination half-life in normal subjects and patients with moderate hepatic impairment.2 Pharmacokinetic data in patients with severe hepatic insufficiency not available.2
Stability
Storage
Sub-Q
Implant
Actions
-
A synthetic decapeptide analog of GnRH; structurally related to leuprolide, nafarelin, and triptorelin.1 2 3 4 5 8
-
A potent inhibitor of gonadotropin secretion when given continuously.1 2 3 4 5
-
Initially, circulating levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH), testosterone, and estradiol surge transiently.1 2 3 4 5 Following chronic and continuous administration (generally, 2–4 weeks after initiation of therapy), produces a sustained decrease in LH and FSH secretion and a marked reduction of testicular and ovarian steroidogenesis.1 2 3 4 5
-
Reductions in serum testosterone concentrations in males receiving goserelin are comparable to those achieved after surgical castration (i.e., <50 ng/dL).1 2 4 5 6 17 Consequently, physiologic functions and tissues dependent on testosterone for maintenance become quiescent.1 2 4
-
In most premenopausal women, serum estradiol concentrations are reduced to levels comparable to those observed after menopause within 3 weeks of initiating therapy.1 3 5 Consequently, physiologic functions and tissues dependent on gonadal steroids (estrogen) for maintenance become quiescent.1 3
Advice to Patients
-
Risk of worsening manifestations of prostate or breast cancer during initial weeks of therapy.1 2
-
Risk of other adverse effects, including decreases in bone mineral density.1 2
-
Risk of diabetes or loss of glycemic control in patients with preexisting diabetes.1 2 23 Importance of undergoing recommended monitoring of blood glucose or HbA1c concentrations.1 2 23
-
Possibility of increased risk of MI, sudden cardiac death, and stroke in men receiving GnRH agonists for the treatment of prostate cancer.1 2 23 Importance of being monitored for manifestations of cardiovascular disease.1 2 23
-
Risk of injection site injury.1 2 Importance of promptly reporting abdominal pain or distension, dyspnea, dizziness, hypotension, and/or altered consciousness.1 2
-
Importance of promptly reporting sudden onset of headache, vomiting, or visual changes to clinician.1 2
-
Necessity of advising women to avoid pregnancy (using nonhormonal contraception) during therapy and for 12 weeks after administration of the last 3.6-mg dose of goserelin.1 If used during pregnancy, advise patient of potential fetal hazard.1
-
Necessity of advising women not to breast-feed.1
-
Importance of women informing their clinician if regular menstruation persists.1 Women also should be advised that breakthrough bleeding or ovulation (with potential for conception) may occur if one or more successive doses of the drug are missed.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1 2
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 2
-
Importance of informing patients of other important precautionary information.1 2 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Implants |
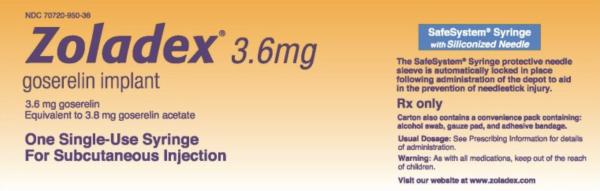
3.6 mg (of goserelin) |
Zoladex (available as prefilled disposable syringe) |
TerSera |
|
10.8 mg (of goserelin) |
Zoladex (available as prefilled disposable syringe) |
TerSera |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 11, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. TerSera Therapeutics. Zoladex, 3.6 mg (goserelin acetate implant) prescribing information. Lake Forest, IL; 2019 Feb.
2. TerSera Therapeutics. Zoladex, 3-month 10.8 mg (goserelin acetate implant) prescribing information. Lake Forest, IL; 2019 Feb.
3. Perry CM, Brogden RN. Goserelin: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in benign gynaecologic disorders. Drugs. 1996; 51:319-46. http://www.ncbi.nlm.nih.gov/pubmed/8808170?dopt=AbstractPlus
4. Brogden RN, Faulds D. Goserelin: a review of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy in prostate cancer. Drugs Aging. 1995; 6:324-43. http://www.ncbi.nlm.nih.gov/pubmed/7613021?dopt=AbstractPlus
5. Cockshott ID. Clinical pharmacokinetics of goserelin. Clin Pharmacokinet. 2000; 39:27-48. http://www.ncbi.nlm.nih.gov/pubmed/10926349?dopt=AbstractPlus
6. Fernandez del Moral P, Dijkman GA, Debruyne FM et al. Three-month depot of goserelin acetate: clinical efficacy and endocrine profile: Dutch South East Cooperative Urological Group. Urology. 1996; 48:894-900. http://www.ncbi.nlm.nih.gov/pubmed/8973673?dopt=AbstractPlus
7. Pilepich MV, Krall JM, al-Sarraf M et al. Androgen deprivation with radiation therapy compared with radiation therapy alone for locally advanced prostatic cancer: a randomized comparative trial of the Radiation Therapy Oncology Group. Urology. 1995; 45:616-23. http://www.ncbi.nlm.nih.gov/pubmed/7716842?dopt=AbstractPlus
8. Bolla M, Gonzalez D, Warde P et al. Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N Engl J Med. 1997; 337:295-300. http://www.ncbi.nlm.nih.gov/pubmed/9233866?dopt=AbstractPlus
9. Prostate Cancer. From: PDQ. Physician data query (database). Bethesda, MD: National Cancer Institute; 2002 Jul.
10. Pilepich MV, Caplan R, Byhardt RW et al. Phase III trial of androgen suppression using goserelin in unfavorable-prognosis carcinoma of the prostate treated with definitive radiotherapy: report of Radiation Therapy Oncology Group Protocol 85-31. J Clin Oncol. 1997; 15:1013-21. http://www.ncbi.nlm.nih.gov/pubmed/9060541?dopt=AbstractPlus
11. Rock JA, Truglia JA, Caplan RJ et al. Zoladex (goserelin acetate implant) in the treatment of endometriosis: a randomized comparison with danazol. Obstet Gynecol. 1993; 82:198-205. http://www.ncbi.nlm.nih.gov/pubmed/8336864?dopt=AbstractPlus
12. Shaw RW. An open randomized comparative study of the effect of goserelin depot and danazol in the treatment of endometriosis. Fertil Steril. 1992; 58:265-72. http://www.ncbi.nlm.nih.gov/pubmed/1386029?dopt=AbstractPlus
13. Taylor CW, Green S, Dalton WS et al. Multicenter randomized clinical trial of goserelin versus surgical ovariectomy in premenopausal patients with receptor-positive metastatic breast cancer: an intergroup study. J Clin Oncol. 1998; 16:994-9. http://www.ncbi.nlm.nih.gov/pubmed/9508182?dopt=AbstractPlus
14. Bajetta E, Zilembo N, Buzzoni R et al. Goserelin in premenopausal advanced breast cancer: clinical and endocrine evaluation of responsive patients. Oncology. 1994; 51:262-9. http://www.ncbi.nlm.nih.gov/pubmed/8196909?dopt=AbstractPlus
15. Breast Cancer. From: PDQ. Physician data query (database). Bethesda, MD: National Cancer Institute; 2002 Jul.
16. Donnez J, Vilos G, Gannon MJ et al. Goserelin acetate (Zoladex) plus endometrial ablation for dysfunctional uterine bleeding: a large randomized, double-blind study. Fertil Steril. 1997; 68:29- 36. http://www.ncbi.nlm.nih.gov/pubmed/9207580?dopt=AbstractPlus
17. Cersosimo RJ, Carr D. Prostate cancer: current and evolving strategies. Am J Health-Syst Pharm. 1996; 53:381-96. http://www.ncbi.nlm.nih.gov/pubmed/8673658?dopt=AbstractPlus
18. Relative effectiveness and cost-effectiveness of methods of androgen suppression in the treatment of advanced prostatic cancer. Summary, Evidence Report/Technology Assessment (No. 4). Agency for Health Care Policy and Research, Rockville, MD. 1999 Jan. http://www.ahrq.gov/clinic/prossumm.htm
19. American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins. Medical management of endometriosis. Practice Bulletin No. 11. Washington, DC: American College of Obstetricians and Gynecologists; 1999 Dec.
20. Schering. Eulexin (flutamide) capsules prescribing information. Kenilworth, NJ; 1999 Sept.
21. AstraZeneca, Wilmington, DE: personal communication.
22. Food and Drug Administration. GnRH agonists: safety review of drug class used to treat prostate cancer (sold under the brand names Lupron, Zoladex, Trelstar, Viadur, Vantas, Eligard, Synarel, and generics). Rockville, MD; 2010 May 3. From FDA web site/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm210576.htm). https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm210576.htm)
23. Food and Drug Administration. GnRH agonists: label change--increased risk of diabetes and cardiovascular disease (update). Rockville, MD; 2010 Oct 20. From FDA web site/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm230359.htm). https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm230359.htm)
10010. Francis PA, Regan MM, Fleming GF et al. Adjuvant ovarian suppression in premenopausal breast cancer. N Engl J Med. 2015; 372:436-46. http://www.ncbi.nlm.nih.gov/pubmed/25495490?dopt=AbstractPlus
10011. Pagani O, Regan MM, Walley BA et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med. 2014; 371:107-18. http://www.ncbi.nlm.nih.gov/pubmed/24881463?dopt=AbstractPlus
10012. Francis PA, Pagani O, Fleming GF et al. Tailoring Adjuvant Endocrine Therapy for Premenopausal Breast Cancer. N Engl J Med. 2018; 379:122-137. http://www.ncbi.nlm.nih.gov/pubmed/29863451?dopt=AbstractPlus
10013. Tevaarwerk AJ, Wang M, Zhao F et al. Phase III comparison of tamoxifen versus tamoxifen plus ovarian function suppression in premenopausal women with node-negative, hormone receptor-positive breast cancer (E-3193, INT-0142): a trial of the Eastern Cooperative Oncology Group. J Clin Oncol. 2014; 32:3948-58. http://www.ncbi.nlm.nih.gov/pubmed/25349302?dopt=AbstractPlus
10016. Pan K, Bosserman LD, Chlebowski RT. Ovarian Suppression in Adjuvant Endocrine Therapy for Premenopausal Breast Cancer. J Clin Oncol. 2019; 37:858-861. http://www.ncbi.nlm.nih.gov/pubmed/30742565?dopt=AbstractPlus
10017. Burstein HJ, Lacchetti C, Anderson H et al. Adjuvant Endocrine Therapy for Women With Hormone Receptor-Positive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update on Ovarian Suppression. J Clin Oncol. 2016; 34:1689-701. http://www.ncbi.nlm.nih.gov/pubmed/26884586?dopt=AbstractPlus
10018. Burstein HJ, Lacchetti C, Anderson H et al. Adjuvant Endocrine Therapy for Women With Hormone Receptor-Positive Breast Cancer: ASCO Clinical Practice Guideline Focused Update. J Clin Oncol. 2019; 37:423-438. http://www.ncbi.nlm.nih.gov/pubmed/30452337?dopt=AbstractPlus
10020. Dowsett M, Lønning PE, Davidson NE. Incomplete Estrogen Suppression With Gonadotropin-Releasing Hormone Agonists May Reduce Clinical Efficacy in Premenopausal Women With Early Breast Cancer. J Clin Oncol. 2016; 34:1580-3. http://www.ncbi.nlm.nih.gov/pubmed/26729430?dopt=AbstractPlus
10023. Gnant M, Mlineritsch B, Stoeger H et al. Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol. 2011; 12:631-41. http://www.ncbi.nlm.nih.gov/pubmed/21641868?dopt=AbstractPlus
10024. Gnant M, Mlineritsch B, Stoeger H et al. Zoledronic acid combined with adjuvant endocrine therapy of tamoxifen versus anastrozol plus ovarian function suppression in premenopausal early breast cancer: final analysis of the Austrian Breast and Colorectal Cancer Study Group Trial 12. Ann Oncol. 2015; 26:313-20. http://www.ncbi.nlm.nih.gov/pubmed/25403582?dopt=AbstractPlus
10025. Bellet M, Gray KP, Francis PA et al. Twelve-Month Estrogen Levels in Premenopausal Women With Hormone Receptor-Positive Breast Cancer Receiving Adjuvant Triptorelin Plus Exemestane or Tamoxifen in the Suppression of Ovarian Function Trial (SOFT): The SOFT-EST Substudy. J Clin Oncol. 2016; 34:1584-93. http://www.ncbi.nlm.nih.gov/pubmed/26729437?dopt=AbstractPlus
10026. Perrone F, De Laurentiis M, De Placido S et al. Adjuvant zoledronic acid and letrozole plus ovarian function suppression in premenopausal breast cancer: HOBOE phase 3 randomised trial. Eur J Cancer. 2019; 118:178-186. http://www.ncbi.nlm.nih.gov/pubmed/31164265?dopt=AbstractPlus
10027. Chlebowski RT, Pan K, Col NF. Ovarian suppression in combination endocrine adjuvant therapy in premenopausal women with early breast cancer. Breast Cancer Res Treat. 2017; 161:185-190. http://www.ncbi.nlm.nih.gov/pubmed/27785653?dopt=AbstractPlus
10028. AHFS final determination of medical acceptance: Off-label use of endocrine therapy in combination with ovarian suppression for the adjuvant treatment of early-stage hormone receptor-positive breast cancer in premenopausal women. Published January 4, 2021.
More about goserelin
- Check interactions
- Compare alternatives
- Reviews (103)
- Side effects
- Dosage information
- During pregnancy
- Drug class: gonadotropin releasing hormones
- En español