Dvorah Dosage
Generic name: ACETAMINOPHEN 325mg, CAFFEINE 30mg, DIHYDROCODEINE BITARTRATE 16mg
Dosage form: tablet
Drug class: Narcotic analgesic combinations
Medically reviewed by Drugs.com. Last updated on Nov 7, 2023.
Important Dosage and Administration Instructions
Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see WARNINGS].
Initiate the dosing regimen for each patient individually, taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see WARNINGS].
Monitor patients closely for respiratory depression, especially within the first 24-72 hours of initiating therapy and following dosage increases with DVORAH and adjust the dosage accordingly [see WARNINGS].
Initial Dosage
Initiating treatment with DVORAH
The usual adult dosage is two (2) DVORAH tablets orally every four (4) hours, as needed. No more than five (5) doses, or ten (10) tablets should be taken in a 24-hour period.
Conversion from Other Opioids to DVORAH
There is inter-patient variability in the potency of opioid drugs and opioid formulations. Therefore, a conservative approach is advised when determining the total daily dosage of DVORAH. It is safer to underestimate a patient’s 24-hour DVORAH dosage than to overestimate the 24-hour DVORAH dosage and manage an adverse reaction due to overdose.
Titration and Maintenance of Therapy
Individually titrate DVORAH to a dose that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving DVORAH to assess the maintenance of pain control and the relative incidence of adverse reactions, as well as monitoring for the development of addiction, abuse, or misuse [see WARNINGS]. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration.
If the level of pain increases after dosage stabilization, attempt to identify the source of increased pain before increasing the DVORAH dosage. If unacceptable opioid-related adverse reactions are observed, consider reducing the dosage. Adjust the dosage to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
Safe Reduction Discontinuation of DVORAH
Do not abruptly discontinue DVORAH in patients who may be physically dependent on opioids. Rapid discontinuation of opioid analgesics in patients who are physically dependent on opioids has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid
discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse. Patients may also attempt to treat their pain or withdrawal symptoms with illicit opioids, such as heroin, and other substances.
When a decision has been made to decrease the dose or discontinue therapy in an opioid-dependent patient taking DVORAH, there are a variety of factors that should be considered, including the dose of DVORAH the patient has been taking, the duration of treatment, the type
of pain being treated, and the physical and psychological attributes of the patient. It is important to ensure ongoing care of the patient and to agree on an appropriate tapering schedule and follow-up plan so that patient and provider goals and expectations are clear and realistic. When opioid analgesics are being discontinued due to a suspected substance use disorder, evaluate and treat the patient, or refer for evaluation and treatment of the substance use disorder. Treatment should include evidence-based approaches, such as medication assisted treatment of opioid use disorder. Complex patients with co-morbid pain and substance use disorders may benefit from referral to a specialist.
There are no standard opioid tapering schedules that are suitable for all patients. Good clinical practice dictates a patient-specific plan to taper the dose of the opioid gradually. For patients on DVORAH who are physically opioid-dependent, initiate the taper by a small enough increment (e.g., no greater than 10% to 25% of the total daily dose) to avoid withdrawal symptoms, and proceed with dose-lowering at an interval of every 2 to 4 weeks. Patients who have been taking opioids for briefer periods of time may tolerate a more rapid taper.
It may be necessary to provide the patient with lower dosage strengths to accomplish a successful taper. Reassess the patient frequently to manage pain and withdrawal symptoms, should they emerge. Common withdrawal symptoms include restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. If withdrawal symptoms arise, it may be necessary to pause the taper for a period of time or raise the dose of the opioid analgesic to the previous dose, and then proceed with a slower taper. In addition, monitor patients for any changes in mood, emergence of suicidal thoughts, or use of other substances.
When managing patients taking opioid analgesics, particularly those who have been treated for a long duration and/or with high doses for chronic pain, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper. A multimodal approach to pain management may optimize the treatment of chronic pain, as well as assist with the successful tapering of the opioid analgesic [see WARNINGS/ Withdrawal, DRUG ABUSE AND DEPENDENCE].
More about Dvorah (acetaminophen / caffeine / dihydrocodeine)
- Check interactions
- Compare alternatives
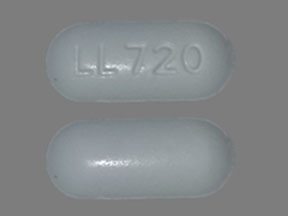
- Drug images
- Side effects
- During pregnancy
- Drug class: narcotic analgesic combinations
Patient resources
Other brands
Trezix, Panlor, Panlor DC, Panlor SS, Zerlor
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.